Paraganglioma of the Carotid Glomus
Rabileh Madina*, Sidki Kenza, Insumbo Paulino, Wen-Yam Traoré, Lanjerie Safae, Saleheddine Tariq, Edderai Meryem and El Fenni Jamal
Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Received Date: 23/07/2024; Published Date: 15/10/2024
*Corresponding author: Rabileh Madina, Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Abstract
Paragangliomas are rare tumors, most often located in the head and neck, can be either sporadic or genetic in origin. Carotid chemodectomas are paragangliomas developed from the carotid glomus, a chemoreceptive structure located in the adventitia of the carotid bifurcation. They are mostly asymptomatic. These tumors have slow growth but tend to invade neighboring structures (carotid vessels and cranial nerves). The diagnosis is relatively simple both clinically and through imaging techniques. Various medical imaging techniques are used to diagnose and pre-treat paragangliomas, as well as to propose appropriate and standardized patient management. Surgical removal is the primary treatment for carotid paragangliomas. The difficulty of tumor removal varies, with radiotherapy and systemic therapy being alternatives in some cases.
We report the case of a 42-year-old female patient who presented with a left lateral cervical swelling without associated clinical signs. The diagnosis of carotid paraganglioma was confirmed by Angio-CT of the neck and cervical MR angiography. This tumor was successfully surgically removed without complications. Based on this observation, our aim is to highlight this generally benign rare condition, describing the different clinical and pathological aspects, illustrating the crucial role of imaging in the assessment of these tumors, and discussing the therapeutic management.
Keywords: Paraganglioma; Chemodectoma; Carotid; Shamblin classification
Introduction
Paraganglioma or chemodectoma of the carotid body is a relatively rare hypervascularized neoplasm, originating from chromaffin cells derived from neuroendocrine cells of the neural crest. It is mostly benign, but certain genetic mutations (SDHB) can be associated with malignant forms. This tumor develops from the carotid body, a chemoreceptor structure located in the adventitia of the carotid bifurcation, and can be sporadic or familial, solitary or multifocal. Carotid paraganglioma accounts for 60-70% of paragangliomas in the cervico-encephalic region. The diagnosis is relatively easy both clinically and paraclinically and It clinically presents itself as a lateral or antero-cervical mass.. It can metastasize locally (to lymph nodes) and distantly (mainly to bones), which is the only criterion for malignancy as histology is not conclusive. The various bilateral carotid imaging techniques provide a diagnosis in nearly 100% of cases by revealing a highly vascularized tumor that expands the carotid bifurcation. The Shamblin classification is based on the encasement of carotid vessels and is correlated with the risk of postoperative vascular injuries occurrence.. Surgery is essentially the main treatment and should be performed in the early stage of development to prevent complications related to tumor growth and those resulting from the intervention. Surgery may be preceded by embolization in order to reduce intraoperative hemorrhagic losses caused by the significant vascularization of the tumor. Radiotherapy complements surgical treatment in cases of lymph node metastases, recurrence after surgery, or incomplete resection. Late recurrences (sometimes several years after the initial resection) are observed in about 5% of cases, and these patients should receive careful follow-up.
Case Report
42 year-old female patient with no particular personal or family pathological history, presents with a progressively increasing left latero-cervical mass without any other associated symptoms. The symptomatology has been evolving for 4 years without any alteration in general condition. The examination of the neck revealed a left latero carotid swelling of 3 cm in size, firm, painless, slightly movable laterally compared to deep planes and skin. There were no palpable cervical lymph nodes. The thyroid gland, submaxillary, and parotid glands were unremarkable.The rest of the somatic examination was normal. Given the pulsatile nature of the mass, an ultrasound of the supraaortic trunks (TSA) was requested, showing a well-defined echogenic oval tissue mass measuring 29x 27x 31mm, well vascularized at the level of the carotid bifurcation. Cervical CT scan examination confirms the origin of the glomus of the tumor at the level of the left carotid bifurcation with a long axis parallel to the vascular axis, classified stage II according to the Shamblin classification, which enhances intensely after contrast (Figure 1). In angio-MRI cervical, the tumor presents in T1 isosignal, T2 hypersignal, with a lyre-shaped image and a salt-and-pepper appearance with arterial vascular contrast enhancement, restriction to the diffusion. This mass widened the carotid bifurcation and pushed back the proximal part of its internal and external branches, extending to the height of C2 to C4 (Figure 2). This is a paraganglioma for which resection is indicated. Excision of the tumor was performed while preserving the carotid arteries with uncomplicated operative outcomes. The patient presents neither local recurrence nor distant metastasis, 12 months after diagnosis.
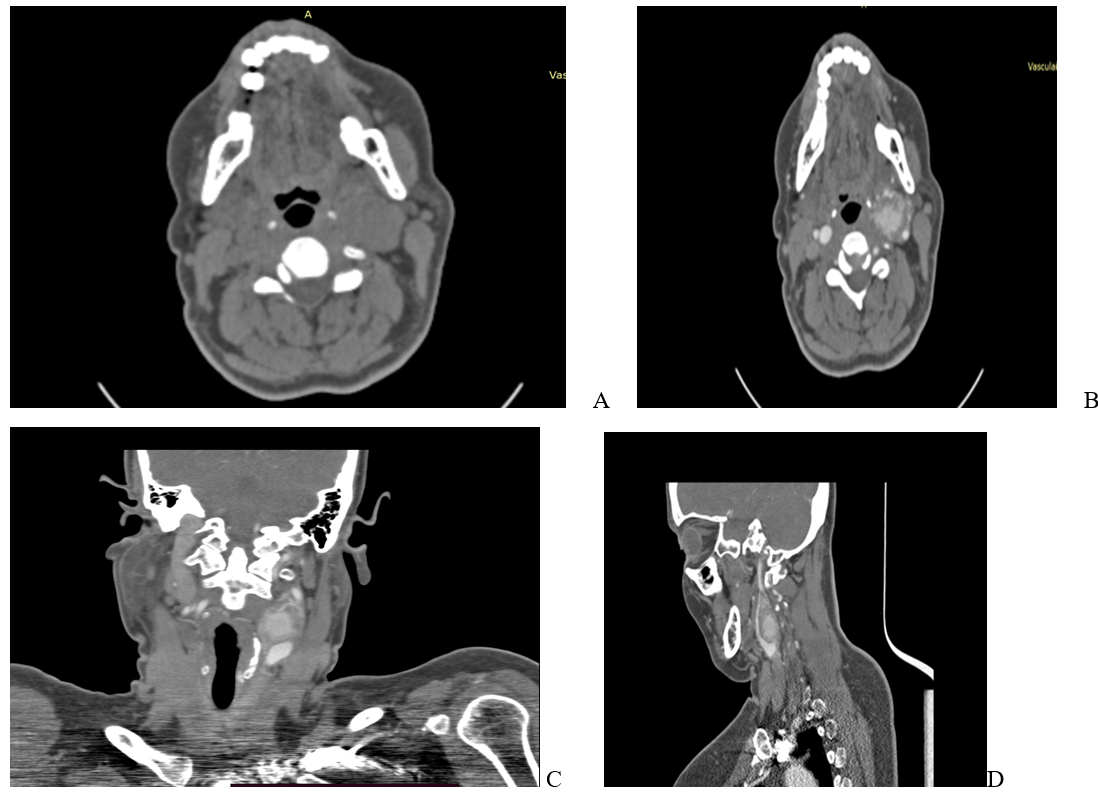
Figure 1: Cervical CT scan in axial section, without contrast agent, (A) objective a homogeneous tissue mass, with clear contours, of average tissue density ,of the left carotid bifurcation, les images B axial ,C coronal ,D sagital which after contrast shows a hypervascularized mass measuring 27x29 mm, this mass widened the carotid bifurcation and pushed back the proximal part of its internal and external branches.

Figure 2: (A) Axial T1-weighted MR image showing left carotid mass with isointense compared to muscle , salt and pepper appearance when larger, representing a combination of punctate regions of hemorrhage or slow flow (salt) and flow voids (arrow). (B) axial T2 weighted MR demonstrating the left carotid paraganglioma (arrow) with high T2-weighted signal intensity compared to muscle with a lyre-shaped image and salt and pepper appearance. (C) restriction to the diffusion. (D) Gadolinium-enhanced axial T1-weighted fat saturated MR image of the tumour showing with arterial vascular contrast enhancement, Note the splaying of the internal and external carotid arteries (arrowheads).
Discussion
Paragangliomas are rare hypervascularized tumors, arising from chromaffin cells which derive from neuroendocrine cells originating from the neural crest. These cells are involved in the production, storage, metabolism and secretion of catecholamines. There is a strong affinity of catecholamines for chromium salts; thus these cells turn brown in their presence, hence their name chromaffins. These cells can be located outside the adrenal medulla at the level of structures belonging to the para- and orthosympathetic system. Paragangliomas are rare tumors; they represent 0.03% of all neoplasias and 0.6% of head and neck .tumors carotid paragangliomas represent (60-70%) paragangliomas of the head and neck Familial forms account for 10% of cases [11,12]. Lesions are bilateral in 40% of cases [11]. Multiple localizations of paragangliomas are found in about 4% of sporadic forms and 30% of hereditary forms, or approximately 20% for all forms combined. There is a predominance of females in most of the series, the sex ratio Female to Male is very variable from one series to another .The very vascular and locally invasive nature of carotid paragangliomas is the cause of clinical symptoms which develop insidiously and depend on the volume of the tumor. A large number of paragangliomas are initially asymptomatic and slow growing. Clinical manifestations are most often linked to the anatomical location of the tumors, by irritation or compression of adjacent structures. The most described are pulsatile tinnitus, cervical swelling, paralysis of certain cranial nerves and hypoacusis. They are sometimes associated with signs of hypersecretion of catecholamine with high blood pressure, and paroxysmal episodes of headache, sweating and palpitations. Several differential diagnoses must be ruled out when faced with a lateralized neck mass, including lymphoma, carotid aneurysm, metastatic lymphadenopathy, thyroid lesion, sublingual gland tumor and “Brachial cleft cysts”. The ultrasound appearance of carotid paragangliomas is that of a heterogeneous, hypoechoic mass located in the carotid bifurcation [7,16,17]. Differential ultrasound diagnosis with other cervical tumors, particularly certain highly vascular lymphadenopathies, can be difficult. It is therefore an examination which allows a certaine orientation. Any vascularized cervical tumor on ultrasound should be evaluated by other imaging examinations. The CT scan provides information on the vascular nature of the tumor, its location, its relationship with neighboring elements as well as possible intracranial infiltration and the presence of a contralateral paraganglioma [16]. It ensures precise analysis of the tumor by defining morphological and topographical characteristics [2,9]. The paraganglioma appears as a homogeneous tissue mass, with clear contours, of average tissue density. During iodine injection, the contrast is rapid, intense and fleeting due to vascular washing phenomena. The distinction of the carotid vessels can be difficult when they are encompassed by a corpuscular tumor [7,9] Concerning MRI angiography, it is the examination of choice and gives a precise evaluation of the locoregional extension and a analysis of the Willis polygon by making cuts in the three planes of space in the event that clamping or ligation of the caortid would be necessary, the diagnosis can be made in the face of hypervascularization of the tumors thanks to angiography sequences in multiplanar sectionsand we find a signal T1 iso to hypointense compared to muscle salt and pepper appearance when larger, representing a combination of punctate regions of hemorrhage or slow flow (salt) and flow voids (pepper) and intense enhancement following gadolinium. T2 hyperintense compared to muscle salt and pepper appearance.The sensitivity of this examination is 90% (12), which allows better detection than angio-CT. On the other hand, this examination is less effective in describing bone damage and hypotympanic lesions. The therapeutic attitude seems to be unequivocal, both in surgical resection and However, radiotherapy can be recommended preoperatively for large tumors or to treat metastases and tumor recurrences.In 1991 Shamblin et al introduced a classification based on tumor size to codify therapeutic conduct. Thus, these tumors are subdivided into three classes:
- Class I corresponds to a small tumor allowing excision outside the carotid vessels;
- Class II includes medium-sized tumors with close vascular relationships requiring subadventitial dissection;
- Finally, class III where the tumor is large and closely linked to the vascular axis requiring resection or replacement of the internal and or external carotid artery.
Conclusion
They require early diagnosis and adequate multidisciplinary management by surgeons, oncologists and radiotherapists depending on the stage. However, reported metastases have proven the possible malignancy of paragangliomas. The diagnosis is suggested based on clinical and angiographic data and confirmed by histopathological examination and immunohistochemical study. Surgery remains the reference curative treatment. Radiotherapy is only used in the case of recurrence, inextirpable tumor or surgical contraindication.
References
- Bougrine F, Maamouri F, Doghri R, Msakni I, Sabbegh Znaidi N, et al. Une tumeur rare du glomus carotidien. Journal des Maladies Vasculaires, 2008; 33(4-5): 214-217.
- Drissia M, Lamrania Y, Maaroufia M, Essatarab Y, Kanjaa N, et al. Masse cervicale chez un adulte. Feuillets de radiologie, 2010; 50(5): 268-272.
- Roden D, Myssiorek D. Prise en charge cervicale des paragangliomes malins de la tête et du cou. Techniques opératoires en oto-rhino-laryngologie, 2016; 27(1): 41-46.
- Alaoui M, Bouzarwata A, El Idrissi R, Benzirare A, Sedki N, Sefiani Y, et al. Paragangliomes multiples : à propos de deux cas. Arch Mal Coeur Vaiss, 2007; 100: 582-586.
- Pellitteri PK, Rinaldo A, Myssiorek D, Gary Jackson C, Bradley PJ, Devaney KO, et al. Paragangliomes de la tête et du cou. Oncologie orale, 2004; 40: 563-575.
- Fakhry N, Niccoli-Sire P, Barlier-Seti A, Giorgi R, Giovanni UN, Zanaret M. Cervicalparagangliomes :estSDHgénétique analyse systématique requise ? Eur Arch Otorhinolaryngol, 2008; 265: 557-563.
- Biller HF, Lawson W, Som P, Rosenfeld R. Tumeurs du glomus vagal. Ann Otol Rhinol Laryngol, 1989; 98: 21-26
- Barbara Peric, Ziva Pohar Marinsek, Breda Skrbinc, Maja Music, Ivana Zagar, et al. Une patiente atteinte d'une tumeur indolore du cou révélée comme étant un paragangliome carotidien : rapport de cas. World J Surg Oncol, 2014; 12: 267-271.
- McCaffrey TV, Myssiorek D, Marrinan M. Paragangliomes de la tête et du cou : physiologie et biochimie. Otolaryngol Clin North Am, 2001; 34(5): 837-844.
- Papaspyrou K, Mewes T, Rossmann H, Fottner C, Brigitte Schneider-Raetzke, et al. Paragangliomes de la tête et du cou : rapport de 175 patients (1989-2010). Tête Cou, 2012; 34(5): 632-637.
- Amato A, Bianco T, Compagna R, Siano M, Esposito G, et al. Résection chirurgicale des paragangliomes du corps carotidien : 10 ans d'expérience. The American Journal of Surgery, 2014; 207(2): 293-298.

