The Dide -Botcazo Syndrome, An Atypical and Rare Presentation of Posterior Cerebral Artery Infarction
Rabileh Madina*, Sidki Kenza, Wen-Yam Traoré, Lanjerie Safae, Zamani Ouijdane and Saleheddine Tariq
Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Received Date: 23/07/2024; Published Date: 15/10/2024
*Corresponding author: Rabileh Madina, Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Abstract
Dide-Botcazo syndrome is a rare neuropsychological disorder characterized by a combination of cortical blindness with anosognosia of blindness, amnesia and topographical disorientation, secondary to bilateral lesions of the occipital cortex also involving the structure of the infero-medial temporal lobe.
We report the clinical case of a 76-year-old man, hypertensive and diabetic ATCD, who presented a picture of cortical blindness associated with anterograde amnesia all without anosognosia followed after a few days by right hemiparesis and the cortical blindness progressed , towards a visual agnosia table .The CT scan revealed a moderately hypodense area without signs of hemorrhagic infarction in the territory of the bilateral posterior cerebral arteries in relation to a bilateral posterior cerebral infarction. The scan also ruled out malformations such as aneurysms or cerebral masses, as well as hemorrhagic stroke. Patient was treated with antiplatelet drugs and early rehabilitation. The progression was marked by a partial improvement in motor disorders and confusion. Cortical blindness and anosognosia were permanent.
Introduction
Dide Botcazo syndrome, also known as DB syndrome, is a rare and not well-known medical condition that involves a mix of neurological symptoms and mental health issues [5,7]. These symptoms can be intermittent and fluctuate in a way that makes the diagnosis and management of this condition complex. This clinical entity was first reported in 1902 by French neurologists Dide, Botcazo, and their colleagues, and since then, only a limited number of cases have been described in the medical literature. Diagnostic approaches often rely on excluding other neurological and psychiatric conditions in order to reach a diagnosis of inclusion of DB syndrome. A CT scan or Magnetic Resonance Imaging (MRI) can confirm an infarction in the brain regions supplied by the bilateral posterior cerebral arteries.
Case Report
A 76-year-old patient, hypertensive and diabetic, initially presented with a picture of cortical blindness without a threat response, only able to distinguish between light and darkness, along with anterograde amnesia, all without anosognosia or oculomotor disturbances ,following a few days, there was the onset of right hemiparesis, and cortical blindness progressed to a picture of apperceptive visual agnosia associated with persistent anterograde amnesia and topographic agnosia, all progressing over the past few weeks. Upon admission to the neurology department, the baseline NIHSS score was 9, blood pressure was high (160/100 mmHg), and the ECG was normal. The clinical examination revealed right hemiparesis without any other neurological signs or abnormal mental symptoms detected. A cerebral CT scan was requested as part of the etiological investigation, revealing a moderately hypodense cortico-subcortical area in the temporo-occipital region without hemorrhagic transformation in the territory of the bilateral posterior cerebral arteries, indicative of a subacute ischemic stroke in the territory of the bilateral posterior cerebral arteries (Figure 1).
The patient was treated with antiplatelet medications and early rehabilitation. Progression showed
partial improvement in motor deficits and confusion. Cortical blindness and anosognosia remained permanent.
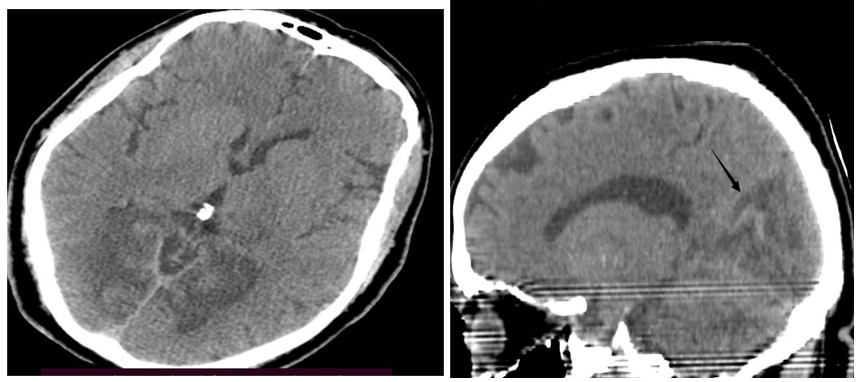
Figure 1: Spontaneous brain CT scan without enhanced contrast, axial y sagital slice, showing moderately hypodense lesion bilateral temporal and occipital cortices of subacute aspect.
Discussion
The posterior cerebral arteries arise from the basilar trunk and branch to supply the medial part of the temporal lobes (including the hippocampus) and the occipital lobes, as well as the thalamus, mammillary bodies, and geniculate bodies. Infarctions in the territory of the posterior cerebral artery occur in about 5 to 10% of all ischemic strokes and present with a wide range of symptoms and clinical signs. However, cortical blindness associated with amnesia is often the result of interaction between the visual cortex, the posterior limbic cortex, and the thalamus via the posterior cerebral artery [6,7]. Cortical blindness results from bilateral destruction of the striate cortex or the optic radiations underlying the cortex [1]. Topographic agnosia is often associated with damage to the parahippocampal gyrus or connections between this area and the visual cortex. Bilateral lesions are necessary to cause severe or persistent memory deficits, particularly through damage to the hippocampus or limbic cortex. Bilateral infarctions of the posterior cerebral artery, including its superficial segments, can also account for cortical blindness [1] Anterograde amnesia is likely associated with lesions in the hippocampus, thalamus, and limbic white matter pathways caused by bilateral posterior cerebral strokes. The posterior cerebral arteries, arising from the basilar trunk and branching to supply the medial part of the temporal lobes (including the hippocampus) and the occipital lobes, as well as the thalamus, mammillary bodies, and geniculate bodies, play a crucial role in the vascularization of these regions associated with memory and vision [1,2,8]. Imaging plays an important role in Dide–botcazo syndrome, allowing for the detection of brain lesions, infarctions, or other structural anomalies that could contribute to the patient's symptoms. In cerebral infarction, a brain CT scan remains essential today to differentiate between a hemorrhagic lesion and an ischemic lesion in the acute phase of cerebral infarctions. Beyond the presence or absence of Intracranial Hemorrhage (ICH), imaging can answer a number of questions regarding the extent of the lesion, its territory, the affected artery, and the mechanism of the stroke. A cerebral angiography allows visualization of the blood vessels in the brain, including the posterior cerebral arteries, and can help identify vascular anomalies such as bilateral infarctions of the PCA [3,4]. The choice of technique depends on its availability and sometimes the possible time delays for its execution.
His neuro-psychosocial prognosis is unfortunately poor, and few therapeutic resources are available. It is differentiated from Anton's syndrome, which associates cortical blindness with anosognosia without medical issues [10,11].
Conclusion
The Dide-Botcazo syndrome is an extremely unique entity characterized by the simultaneous presence of cortical blindness, anosognosia, amnesia, and topographic disorientation, secondary to bilateral occipital and temporal lobe lesions. However, it is crucial to consider the possibility of ischemic stroke if there is manifestation of cortical blindness and amnesia, symptoms which are not typical and can lead to a delay in diagnosis and urgent management.
References
- Barnaud P. Bilateral thromboses of the posterior cerebral artery, Thesis MM. Bordeaux, 1965; p 113.
- Benson DF, Marsden CD, et Meadows JC. The amnesic syndrome of posterior cerebral artery occlusion, Acta Neurol. Scand, 1974; 50: 133-145.
- Lee E, Kang DW, Kwon SU, Kim JS. Posterior cerebral artery infarction:diffusion-weighted MRI analysis of 205 patients. Cerebrovascular Diseases, 2009; 28(3): 298- 305. doi:10.1159/000229016.
- Kim JS, Kim J. Pure midbrain infarction: clinical, radiologic, and pathophysiologic findings. Neurology, 2005; 64(7): 1227-1232.
- De Lorenzo LGL, Di Camillo E, Buiatti T. The Dide–Botcazo syndrome: forgotten and misunderstood. Cortex, 2014; 56: 182-190. http://dx.doi.org/10.1016/j.cortex.2013.01.011.
- Cappellari M, Tomelleri G, Di Matteo A, Carletti M, Magalini A, Bovi P, et al. Dide–Botcazo syndrome due to bilateral occlusion of posterior cerebral artery. Neurological sciences, 2010; 31(1): 99-101. doi:10.1007/s10072-009-0179-7.
- Brandt T, Steinke W, Thie A, Pessin MS, Caplan LR. Posterior Cerebral Artery Territory Infarcts: Clinical Features, Infarct Topography, Causes and Outcome 1 The authors dedicate this paper to Michael S. Pessin, MD, who died before publication. Multicenter Results and a Review of the Literature. Cerebrovascular Diseases, 2000; 10(3): 170-182.
- Brandt T, Thie A, Caplan LR, Hacke W. Infarcts in the brain areas supplied by the posterior cerebral artery. Clinical aspects,pathogenesis and prognosis. Der Nervenarzt, 1995; 66(4): 267-274.
- Yamadori A, Kuromaru S, Tamaki N, Shimoyama T, Takahashi T, Tatsugami H, et al. Dide and Botcazo syndrome—syndrome of bilateral obstruction of posterior cerebral arteries. Psychiatry and Clinical Neurosciences, 1977; 31(4): 619-623.
- Morino K, Yoneda Y, Inaba R, Kita Y, Tabuchi M, Mori E. Dide-Botcazo syndrome associated with Anton's syndrome after a cardioembolic infarction in the distribution of the bilateral posterior cerebral arteries. Rinsho Shinkeigaku= Clinical Neurology, 2002; 42(3): 247-250.
- Yamadori A, Kuromaru S, Tamaki N, Shimoyama T, Takahashi T, Tatsugami H, et al. Dide and Botcazo syndrome of bilateral obstruction of posterior cerebral arteries. Psychiatry and Clinical Neurosciences, 1977; 31(4): 619-623.

