A Case Report on Breast Filariasis- an Incidental Finding on FNA Smear
Surendra Kumar1,*, Savita Agarwal2, Suha Akhtar2 and Anubhav Gautam2
1Department of Pathology, King George’s, Medical University, Lucknow, Uttar Pradesh, India
2Department of Pathology, Uttar Pradesh University of Medical sciences, India
Received Date: 12/07/2024; Published Date: 14/10/2024
*Corresponding author: Dr. Surendra Kumar, Department of Pathology, King George’s, Medical University, Lucknow, Uttar Pradesh, India
Abstract
Introduction: Filariasis is a major health problem in tropical countries including India and is endemic in states like Uttar Pradesh, Bihar and Jharkhand. Fine needle aspiration cytology plays an important role in prompt recognition of disease. Extra-nodal filariasis is a rare entity, and the breast is also one of the sites for filariasis. Patients commonly present with an underlying lump that may occasionally mimic malignancy. The disease mainly involves the lymphatic system of the body. The most frequently involved lymphatics are those of the lower limbs, retroperitoneal tissues, glands, spermatic cord, and epididymis. Lymphatic filariasis is mostly caused by Wuchereria bancrofti and Brugia malayi. However, filarial breast nodule is a very rare finding even in an endemic region. Here, we present one case of filarial breast lump diagnosed by fine needle aspiration cytology.
Case Series: The present case includes incidentally detected microfilaria in breast aspirates along with the associated underlying breast pathology which we thought to be a fibroadenoma/Benign breast disease.
Conclusion: Filarial breast nodule is rare, and it often mimics a neoplastic breast lesion. FNAC is a very effective diagnostic tool in the diagnosis of filarial breast lesion and it helps avoid unnecessary surgical procedure. It should be considered as a differential diagnosis for short-lasting nodular breast lump, especially in countries like India, where filariasis is an endemic disease.
Keywords: Filaria; Breast; FNAC
Case Scenario in Our Study
A 35-year-old female presented in surgery OPD with a painless breast lump in the left breast for ten days and was sent in our department of pathology, UPUMS, Saifai for FNAC. The lump was painless and non-progressive in size. The patient was non lactating mother and had no history of fever, anorexia, weight loss or nipple discharge. General physical examination was unremarkable. On systemic examination, there was a single well defined, mobile, non-tender lump of size 1.0 x 0.5 cm in upper outer quadrant of left breast. No palpable axillary lymph nodes were present. The overlying and adjacent skin was unremarkable. Ultrasonography revealed a cyst at 1 to 2 O’ clock level- two echoic cystic lesion of size approximately 0.52 x 0.38 cm and 0.24 cm seen in superficial, 2.3 mm deep from skin surface.
Materials and Methods
FNAC was done to evaluate the nature of the lesion. Aspiration was done by a 23 G needle attached with a 5 ml syringe and yielded blood mixed material. Two smears were made out of which one was kept air-dried and stained with May Grunwald Giemsa stain (MGG), another smear was fixed in 95% ethanol and stained with H& E stain. We did not perform wet mount preparation as it was not pre-determined it to be case of filariasis, and in second FNAC pass we did not find any moving microfilaria worms in sampling.
Microscopic Examination
Smears revealed many sheathed adult microfilariae singly and with occasional benign ductal epithelial cells (Smears were hypocellular and showed few foamy histiocytes and multinucleated giant cells also (Figure 1a & b). A second repeat procedure was done on next day to look for any malignant features if any. But the second day FNA reveled a smaller number of microfilariae as compared to the day one attempt. The peripheral blood sample did not show presence of microfilaria with absence of peripheral eosinophilia. A buffy coat was also prepared from the blood sample taken but no microfilaria was found.
She was treated with diethylcarbamazine (DEC) for 3 weeks and the patient was cured of the current problem under follow up period.
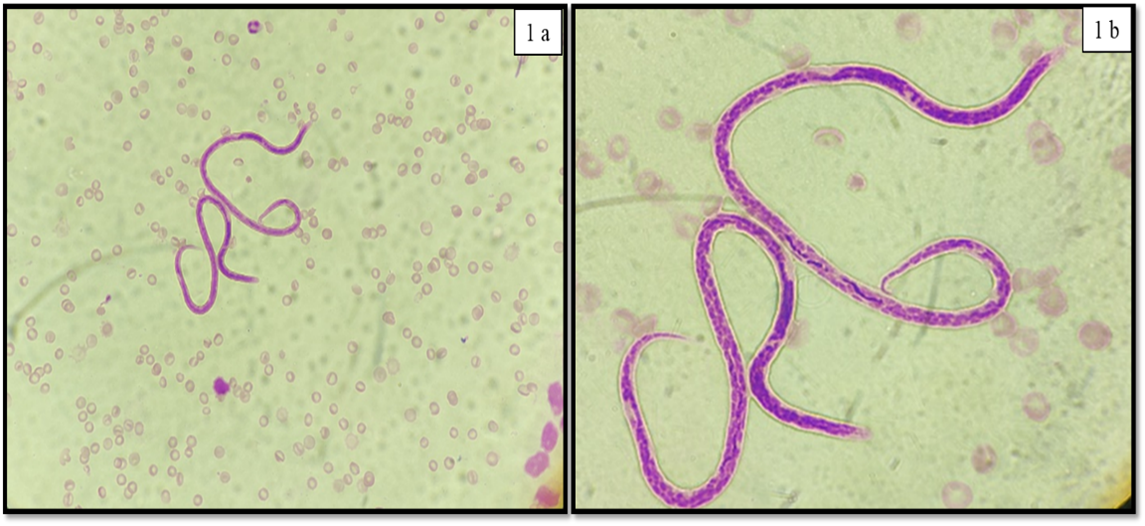
Figure 1: Cytological smear: (a) Two microfilaria adjacent to single neutrophil and lymphocyte (MGG stain, X40 mangnification) (b) Two coiled and sheathed microfilaria (nuclei not extend up to the tip of the tail) (MGG stain, X100 oil immersion).
Discussion
Filarial worms are nematode parasites belonging to the order Spirurida and superfamily Filarioidia. The adult female worms are usually of 80–100 mm length, ovoviviparous giving birth to ova containing microfilariae whereas males are 40 mm in length [1]. Adult worms are found in lymphatic vessels of lower limbs, spermatic cord, epididymis, testis, retroperitoneum and breast of humans, while the larval forms (microflaria) may circulate in the peripheral blood [2].
Filariasis may present as peripheral blood eosinophilia (preferably mid night sampling demonstrate it), lymphangitis and elephantiasis being a lymphatic parasite. It may cause complications like lymphatic obstruction, cystic changes and finally the calcification in the extra-lymphatic tissues. The probable explanation for the mechanism of microflariae reaching extravascular tissue spaces from microcirculation is by crossing the vessel wall by their boring ability [3]. In literature review, there are very few case reports based on accidental findings of filarial worms in FNAC. There are various case reports depending on different sites of FNAC like spermatic cord, epididymis and bone marrow [3-5] apart from breast.
In review of literature, we could find few case reports demonstrating the microfilarial worms on FNAC which are Chakarbarti et al [5] which demonstrated adult filarial worms with many microfilarias in breast lump FNAC in a clinically suspected case of fibroadenosis; Pal et al [6] which demonstrated filarial breast nodule on FNAC without any peripheral blood eosinophilia. Similarly, Satpathi et al [7] and Naorem et al [8] have also presented case reports elaborating microfilaria in breast nodule FNAC.
A case report by Dayal A et al [9] in a 21-year-old female left breast lump presenting with skin induration and inversion of nipple has shown the presence of microfilarias along with granuloma.
Our case was clinically and radiologically unsuspected case of microfilaria and found to be typically an incidental finding of microfilarial worms on breast lump FNAC because we were not sure with the USG report of two cystic lesions turned out to be Filariasis. The differentials we kept in our mind were fibroadenoma with cystic changes or benign cystic lesions or breast abscess.
The role of FNA cytology in the diagnosis of filariasis is well established and cost effective.
The USG breast done at our institute radiology department did not find any moving microfilaria on those two cystic lesions. Infact, a specific movement of worms called as filarial dance has been described by USG in a radiological study by Mashankar A et al [10]. After a period of time these worms calcify and then mammographic findings are indistinguishable from intra-ductal carcinoma of breast [11].
Cytology revealed adult filarial worm having hyaline sheath, cephalic space and presence of somatic cells (nuclei) which appears as granules that extends from the head to the tail. Tail tip is free of nuclei in adult filarial worm of W. bancrofti. Very scant benign ductal epithelial cells along with mixed inflammatory infiltrate (polymorphs, lymphocytes, eosinophils and histiocytes) is also seen. The presence of epithelioid cell granulomas and giant cells is also coincidental finding.
Conclusion
FNAC is a good alternative tool to screen and diagnose such case of incidental finding for Filariasis where we were thinking of the deep subcutaneous nodule to be a case of fibroadenoma. And despite failure to detect any microfilaria in peripheral blood smear with or without associated eosinophilia and buffy coat preparation, the cytological workup may help to reach the diagnosis of the lesion. Although rare finding, still It should be considered as a differential diagnosis for non-subsiding subcutaneous nodular breast lump among the long list of breast lump differentials.
References
- Chatterjee KD. Phylum Nemathelminthes: Class Nematoda. In: Chatterjee KD, editor. Parasitology in relation to clinical medicine. Calcutta: CBS Publishers and distributors, 1980; pp. 237–238.
- Afrose R, Alam MF, Ahmad SS, Naim M. Filarial abscess: aspiration of adult gravid female worm from submandibular region, an unusual presentation. J Cytol, 2017; 34: 66–68. doi: 10.4103/0970-9371.197626.
- Santosh T, Manoj KP, Atanu KB, Anita C. Microfilariae in a bone marrow aspirate. BMC Res Notes, 2016; 9: 256–259. doi: 10.1186/s13104-016-2051-1.
- Mitra SK, Mishra RK, Verma P. Cytological diagnosis of microfilariae in filariasis endemic areas of eastern Uttar Pradesh. J Cytol, 2009; 26: 11–14. doi: 10.4103/0970-9371.51333.
- Chakrabarti I, Das V, Halder B, Giri A. Adult filarial worm in the aspirate from a breast lump mimicking fibroadenosis. Trop Parasitol, 2011; 1: 129–131. doi: 10.4103/2229-5070.86965.
- Pal S, Bose K. Microfilaria in fine needle aspiration cytology of breast lump: an unusual finding. J Health Spec, 2015; 3: 235–237. doi: 10.4103/1658-600X.166491
- Satpathi S, Patnaik J, Rath PK, Panda RR, Behera PK, Satpathi P. Adult filarial worm by fine needle aspiration cytology of breast lumps. Acta Cytol, 2010; 54(5): 10857.
- Naorem GS, Leena C. Filariasis of the breast, diagnosed by fine needle aspiration cytology. Ann Saudi Med, 2009; 29(5): 414–415. doi: 10.4103/0256-4947.55178
- Dayal A, Selvaraju K. Filariasis of The Breast. WebmedCentral Surgery, 2010; 1(11): WMC00942 doi: 10.9754/journal.wmc.2010.00942.
- Mashankar A, Khopkar K, Parihar A, Salkade P. Breast Filariasis. Ind J RadiolImag, 2005; 15: 203-204.
- Friedman PD, Kalisher L. Filariasis. Radiology, 2002; 222: 515-517.

