In Situ Laser Fenestrated EVAR for a Juxtarenal Infective Native Aortic Aneurysm
Daniela Toro, Tomas Ohrlander and Karl Sörelius*
Department of Vascular Surgery, Rigshospitalet, Copenhagen, and Faculty of Health and Medical Sciences, University of Copenhagen, Denmark
Received Date: 05/07/2024; Published Date: 11/10/2024
*Corresponding author: Karl Sörelius, MD, PhD, Department of Vascular Surgery, Rigshospitalet, Copenhagen, and Faculty of Health and Medical Sciences, University of Copenhagen, Denmark
Abstract
Objective: Infective native aortic aneurysms (INAA) is a rare acute condition, which needs to be recognized promptly, to initiate antibiotic therapy and perform surgery. The surgical approach should be tailor-made to each patient taking factors into account as age, comorbidities, prior surgery, sepsis or circulatory chock and aneurysm location, which this case demonstrates.
Methods: This case report describes a 64 years old man, under current antibiotic treatment for pneumococcal meningitis, who developed severe abdominal pain, increase in inflammatory laboratory parameters, and serial computed tomography angiographies demonstrated a juxtarenal INAA, with fast progression.
Results: Urgent surgery was required, and the optimal solution was to perform a 2-in situ laser fenestrated EVAR (ISLF EVAR) for the renal arteries, which was carried out successfully. The patient became asymptomatic, an inflammatory laboratory parameter normalized with continued antibiotic therapy within one month time. Antibiotics was discontinued after a total of six months without any infection-related complications afterwards.
Conclusion: The case demonstrates the immediate applicability of in situ laser fenestrated solutions, when there is neither time for custom made devices, nor possible with an off the shelf solution. This is the first case in the literature to demonstrate a 2-ISLF EVAR for an abdominal INAA.
Keywords: Infective native aortic aneurysm; In situ laser fenestration; EVAR; Mycotic aneurysm; INAA
Introduction
Infective Native Aortic Aneurysms (INAA) develop due to a wide range of bacteria but mainly Salmonella sp., Streptococcus sp., E. coli, and Stapylococcus aureus [1,2]. INAAs may develop through the entire course of the aorta, but the majority of cases develop in the infrarenal aorta [2].
The condition is acute with both a blood stream infection, which may develop to sepsis, and a fast-progressing aortic aneurysm prone to rupture. The diagnosis is made according to the Academic Research Consortium of INAA’s (ARCof INAA) consensus document, through a combination of clinical, laboratory and radiological features with no other diagnosis being more probable [3].
The patients are often old with significant co-morbidities, making surgical treatment very challenging, with both open surgical repair and endovascular aortic repair being equivalent options with their respective pros and cons, why the surgical approach needs to be invidualized [4,5].
In situ laser fenestrated (ISLF) endovascular aortic repair allows for individual customization of a standard aortic stent graft for fenestration (revascularization) of relevant branches of the aorta. The treatment method is relatively new, and most reported cases involve fenestrations of the left subclavian artery, but reports are becoming more frequent on ISLF branches of the visceral aorta for aortic aneurysms [6,7]. The results on short-term are good, but the long-term durability needs further evaluation regarding target vessel patency, development and frequency of endoleak and need for re-intervention.
Case Report
A 64-year-old man with pneumococcal meningitis had been under antibiotic therapy for over a month. His medical history included hypertension, chronic obstructive pulmonary disease, and was an active smoker for 35 years, and had had three years prior suffered a subdural hematoma requiring surgical evacuation with severe ataxia as sequelae.
Suddenly, he presented with acute abdominal pain, fever, elevated white blood cell count (WBCC, from 8.1 to 13.8x109/L) and C-reactive protein (37 to 200 mg/L). Serial contrast enhanced Computed Tomographies (CT) demonstrated a saccular aneurysm with rapid progression just below the left (but at the same level as the right) renal artery with a peri-aortic mass, and a concomitant saccular aneurysm in the left external iliac artery with rapid progression, see Figure 1A and B. The juxtarenal aneurysm measured a maximum diameter of 42 mm, the aorta below was normal with a diameter of 22 mm, and unchanged from a CT one month prior. An 18F-FDG PET-CT visualized focal uptake in both the aneurysms, both with a SUVmax of 18, see Figure 1B. Despite being under directed antibiotic treatment the patient had thus developed two INAAs, and was in severe abdominal pain. The INAAs required urgent repair.
Because of the patient’s relatively young age, serious consideration was taken for OSR. But, OSR was deemed too hazardous due to involvement just below the left renal artery (which is more cranial to the right) and the large periaortic mass, and there was concern regarding the quality of the aorta for making the proximal anastomosis. There was no time for ordering an endovascular Customed-Made Device (CMD).
It was decided, after acquiring informed consent from the patient, to perform an acute ISLF 2-fEVAR.
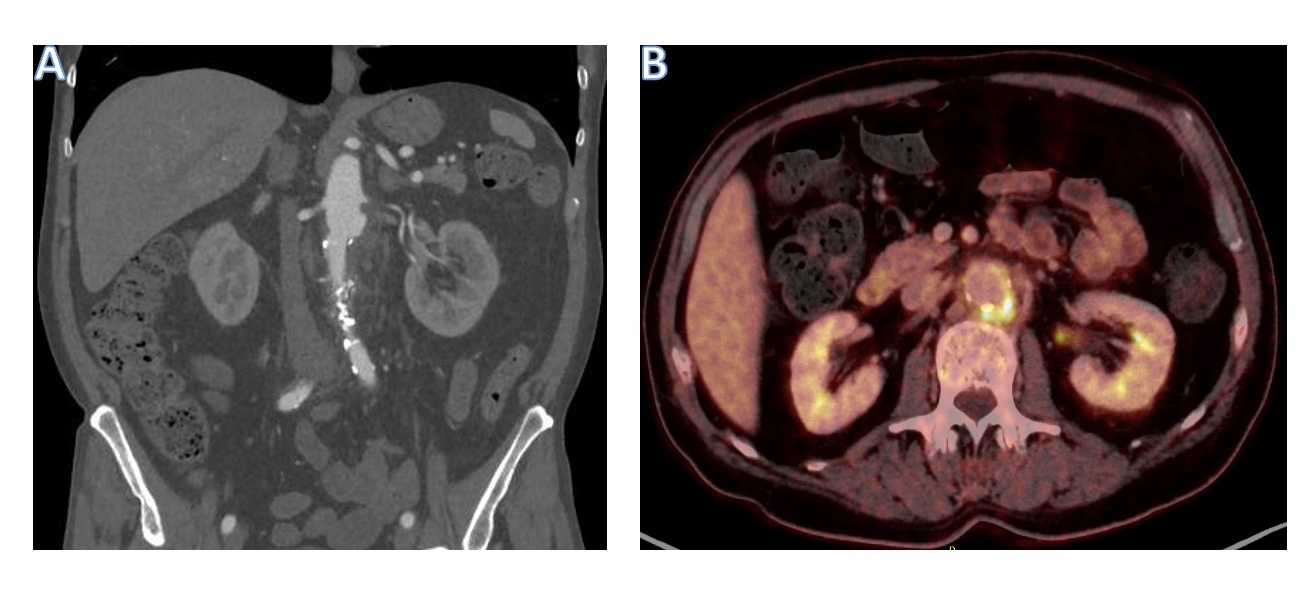
Figure 1A: demonstrate the preoperative CT-angiography findings of a saccular aortic aneurysm, 45 mm in maximum diameter and a peri-aortic mass, and Figure 1B demonstrate the preoperative 18F-FDG PET-CT with focal uptake just below the left renal artery, at the place of the saccular aneurysm. The rest of the aorta was normal.
First, orientation stents were placed flush at the ostium in both renal arteries (Radix2 6-22, Alvimedica). Then a standard EVAR with ESBF 2514C103EE (Medtronic Endurant II stentgraft) was placed just below the superior mesenteric artery (SMA), thus covering both renal arteries, followed by quick bilateral limb extentions for each respective common iliac artery (both ETLW 1616C124EE, Medtronic Endurant II stentgraft). Subsequently, using the 308 Philips Excimer CVX-300 Laser system (Spectranetics, Colorado Springs, CO, USA) and a 0.9 Probe compatible with a 0.018 guidewire (setting Fluency 40 mJ/mm2, 40 pulses/s), laser fenestrations were performed for both the renal arteries with the support of a steerable sheath (Heartspam 8.5 Fr, Merit Medical). Performing the fenestrations took 5 and 12 minutes respectively, and prolonging the total procedure time with 21 minutes. The fenestrations were predilated with a 2-20 and 3-20 mm balloons, inflated to nominal pressures. Then both ISLFs were stent grafted from the aorta into the previously placed orientation renal stents, using BeGraft peripheral 6-22 stentgrafts (Bentley InnoMed GmbH). The BeGrafts were the flared with a 7 mm ballon in the proximal protruding aortic segment. At last, a covered stentgraft 10-80 Viabahn (GORE VIABAHN) was placed in the left external iliac artery.
The final angiography demonstrated complete seal of both the INAAs, without any endoleaks, and normal contrast filling of both the renal arteries and the SMA, see Figure 2A and B.
After four hours observation in the postoperative anaesthesia ward, the patient was transferred to the ward. The patient’s pain subsided within 24 hours, as did the fever, and his inflammatory laboratory values were normalized within three weeks. The patient’s renal laboratory values (creatinine and eGFR), were unaffected the postoperative days. After having completed a month of intravenous directed antibiotic therapy, he was planned for long-term per oral antibiotic treatment in close collaboration with specialists in infectious diseases (minimum six months course). A CT before discharge demonstrated excluded juxtarenal INAA without progression, no endoleak, patent renals arteries, exclusion of the saccular aneurysm of the left iliac artery and significant decrease in periaortic mass. The patient has been monitored with regular clinical examinations and laboratory inflammatory parametres in the out-patient clinic, coupled with CT scans for early detection of infection-related complications as well as for durability of surgery. After six months on antibiotics and the patient had remained asymptomatic, had normal findings on clinical examination, had normal laboratory values (WBCC and CRP), and no sign of IRC on follow-up CT, antibiotics were discontinued. On the last CT scan the saccular aneurysm had completely vanished. The patient is still under clinical, laboratory and imaging surveillance with CT, but all remains normal after a total of 20 months.
The patient gave informed consent for this to be published.
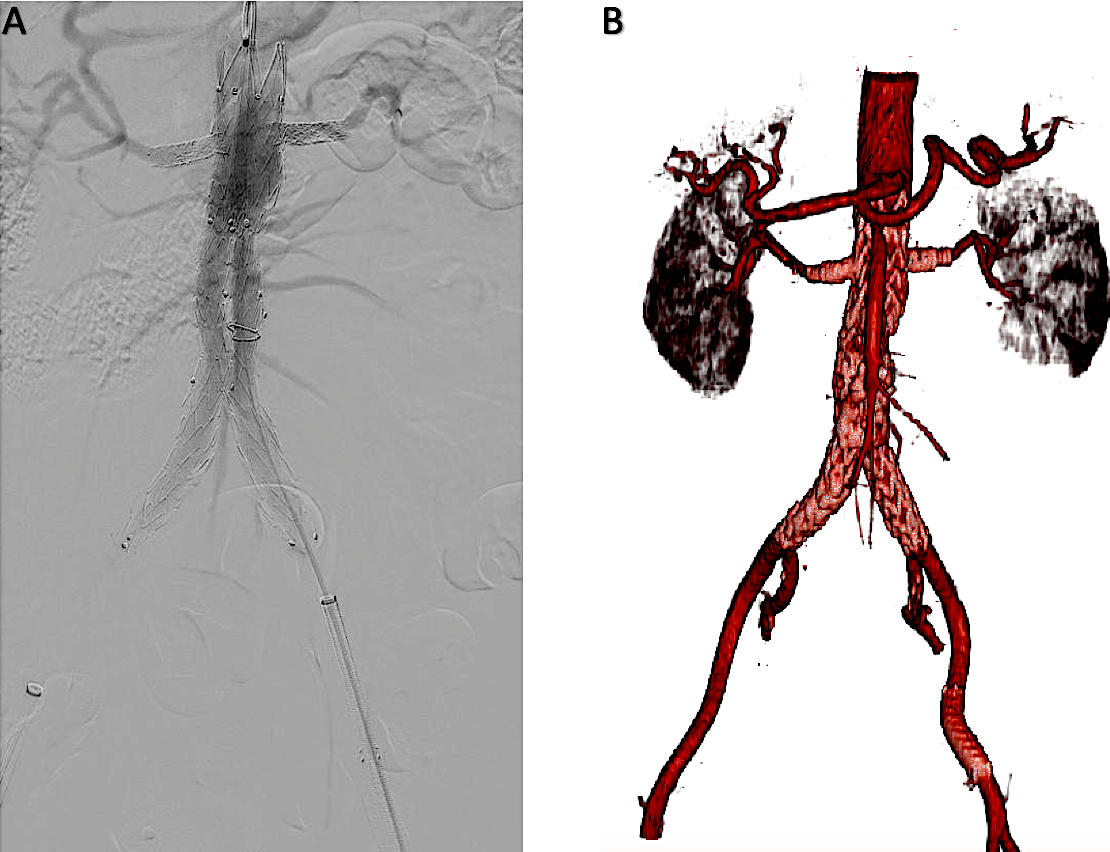
Figure 2A: demonstrate the final angiography with complete seal of both the INAAs, without any endoleaks, and normal contrast filling of both the renal arteries and the SMA. Figure 2B Demonstrate the vessel reconstruction including the 2 in situ laser fenestrated renal stents and the EVAR along with the stentgraft placed in the left external iliac artery.
Discussion
To date, there is only one publication of an ISLF endovascular solution for an INAA, but in the distal aortic arch [8]. This is the first case in the literature to demonstrate a 2-ISLF EVAR solution for an abdominal INAA. The surgery was successful, but the results on long-term needs to be evaluated. As far as the risk of later development of infection-related complications (IRC; postoperative sepsis, development of a vascular graft or endograft infection, new infective aortic aneurysm or aorto-enteric fistulation), it should not however be any greater than that of conventional EVAR [5]. But regarding patency of the target vessels, as well as risk of later tears in the endograft with subsequent endoleak need to be evaluated. An alternative could have been to perform a physician made endograft PMEG), but the experience of this is limited at the treating center, and ISLF solutions being used more often.
The immediate availability, coupled with its flexibility in regards to multiple target vessels with laser fenestrated solutions in complicated acute aortic syndromes is appealing, such as in this case INAAs. The case demonstrates the wide applicability when there is neither time for CMDs, nor possible with an off the shelf solution.
Conclusion
The case demonstrates the immediate applicability of in situ laser fenestrated solutions for acute aortic conditions such as INAA, when there is neither time for custom made devices, nor possible with an off the shelf solution, and when open surgical repair is not an attractive option. However, more research is warranted to evaluate the durability of ISLF for INAAs.
Declaration of interest: None
Prior presentation of case: None
References
- Sörelius K, Budtz-Lilly J, Mani K, Wanhainen A. Systematic Review of the Management of Mycotic Aortic Aneurysms. Eur J Vasc Endovasc Surg, 2019; 58: 426-435.
- Sörelius K, Wanhainen A, Furebring M, Mani K. The Microbiology of Infective Native Aortic Aneurysms in a Population-Based Setting. Ann Vasc Surg, 2022; 78: 112-122.
- Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T, et al. Editor's Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg, 2019; 57: 8-93.
- Sörelius K, Wyss TR, Adam D, Beck AW, Berard X, Budtz-Lilly J, et al. Editor’s Choice - Infective Native Aortic Aneurysms: A Delphi Consensus Document on Terminology, Definition, Classification, Diagnosis, and Reporting Standards. Eur J Vasc Endovasc Surg, 2023; 65: 323-329.
- Wyss TR, Giardini M, Sörelius K. Academic Research Consortium of Infective Native Aortic Aneurysm (ARC of INAA). Infective Native Aortic Aneurysm: a Delphi Consensus Document on Treatment, Follow Up, and Definition of Cure. Eur J Vasc Endovasc Surg, 2024; 67: 654-661.
- Dean A, Wanhainen A, Mani K, Kuzniar M, Grima M, Zuccon G, et al. In Situ Laser Fenestrations of Aortic Endografts for Emergent Aortic Disease. Ann Vasc Surg, 2023; 93: 329-337.
- Glorion M, Coscas R, McWilliams RG, Javerliat I, Goëau-Brissonniere O, Coggia M. A Comprehensive Review of In Situ Fenestration of Aortic Endografts. Eur J Vasc Endovasc Surg, 2016; 52: 787-800.
- Hill MA, Wooster M, Zeigler S. Palliative Repair of a Mycotic Aortic Arch Pseudoaneurysm with a Physician-Modified Endograft and In-Situ Laser Fenestration. J Endovasc Ther, 2022; 29: 132-135.

