Medical Management of Phimosis – Our Experience
Ravitej Singh Bal*, Karanbir Singh, Navdeep Saini and Aakriti Sharma
Department of Surgery, Dr. B.R Ambedkar Institute of Medical Sciences, India
Received Date: 23/06/2024; Published Date: 09/10/2024
*Corresponding author: Ravitej Singh Bal, Department of Surgery, Dr. B.R Ambedkar Institute of Medical Sciences, Mohali, Punjab, India
Introduction
When a prepuce has phimosis, its distal preputial ring is tightly wound, preventing it from retracting. 96% of male new-borns have physiological phimosis. The preputial opening gradually widens to permit normal foreskin retraction in cases where this condition is rarely true phimosis. The incidence drops to 10% by the age of three, and by the age of fourteen, it drops to 1% gradually. Young boys frequently present with preputial adhesions, in which the glans and foreskin are adherent, without the presence of a constricting cicatrix of fibrotic tissue, instead of phimosis. If these adhesions become symptomatic in older boys, gentle foreskin retraction usually resolves them; however, retraction in preschool-aged boys may be traumatizing and should not be done. Boys may exhibit pathological phimosis, a condition in which regular penile hygiene is impeded by a constricting tissue cicatrix. The usual therapy in these cases is circumcision. A history of balanoposthitis episodes or forced retraction with scarring afterward may have resulted in the formation of the cicatrix.
No matter the cause, circumcision has long been the standard of care for pathological phimosis. In recent years, there has been much discussion about the routine practice of circumcision. Despite its effectiveness, this procedure carries a risk of surgical complications such as tissue injury, bleeding, infection, and meatal stenosis. A urethrocutaneous fistula or glans amputation are examples of tissue injury. These wounds might be severe enough to require a significant amount of reconstruction. The risk of anesthesia associated with circumcision, the expense of surgery, and the discomfort experienced during the healing process are additional reasons to try to preserve the foreskin, even though surgical complications are uncommon.
A more conservative approach to phimosis has been described in a number of published reports over the past few years. The application of topical steroids and nonsteroidal anti-inflammatory creams to the phimotic foreskin is supported by these studies. From 67 to 95% of cases are successful, and no negative effects have been noted. We present our initial experience with this conservative approach to phimosis.
Material and Methods
Fifty boys aged one to fourteen who had phimosis presented to our hospital between April and May of 2024. They were given our treatment plan, which consists of cleaning the foreskin with a five percent povidone iodine solution, fomenting it with boric powder, and applying steroidal ointment (0.5 percent betamethasone) twice a day for two weeks. This treatment was only administered to boys whose phimosis was evident from a constricting ring of tissue. Although 5 of the 50 patients experienced preputial ballooning during voiding and 5 had a history of balanoposthitis, the majority of patients were asymptomatic. We excluded from our study any boys younger than a year old or those exhibiting any signs of balanoposthitis at the time of presentation. Patients began a 14-day course of our treatment twice daily, limited to the constricting distal aspect of the foreskin, after the family was counseled regarding treatment options. It was recommended that parents administer the medication rather than patients. Families were advised against pulling the prepuce back with force while applying. We evaluated the foreskin retractability after 14 days. In cases that showed very little or no improvement, treatment was continued for 14 days again and reviewed.
Results
After 14 days, 48 out of the 50 boys were evaluated. Two boys could not be reached when they did not return for a follow-up. Forty (80%) of the 48 patients had a foreskin that appeared normal and easily retracted. The other eight boys had unsuccessful outcomes and were required to undergo 14 additional days of medical therapy. In five boys, phimosis was resolved following a second therapy. Three have undergone circumcision; two did not improve following therapy, and one experienced a recurrence. Pathological examination of the foreskin revealed chronic inflammation and a normal foreskin in 2 boys each. Patients who did not respond well to treatment were older than those who did (mean age 10.6 versus 6.3 years). In a boy who initially had an excellent response, phimosis recurred. He was put back on the regimen, but this time the response was negative and he was circumcised. Four out of the five boys who had previously experienced balanoposthitis had successful outcomes. There were no apparent side effects.
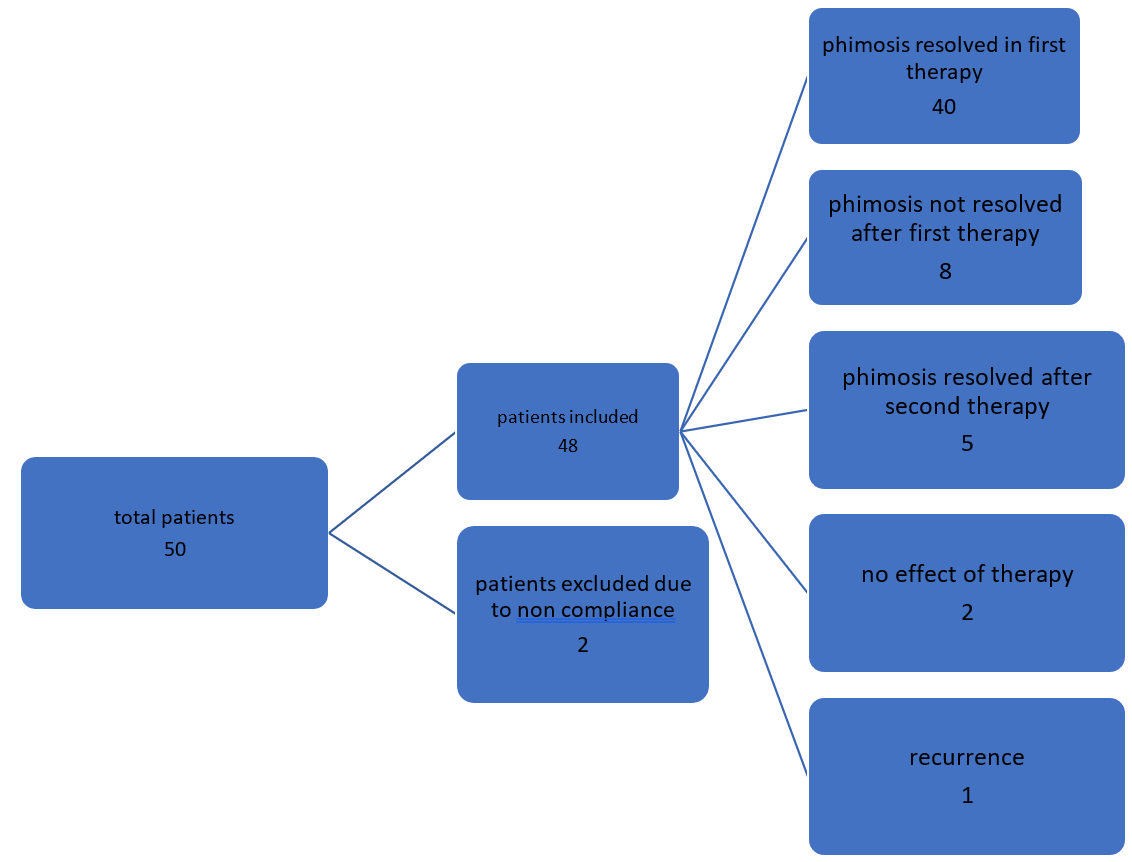
Figure 1: Outcome of the boys with phimosis treated with medical therapy.
Discussion
The incidence of pathological phimosis is 0.4/1000 boys per year; that means only 0.6% of boys are affected by their 15th birthday. This is much lesser than physiological phimosis, which is common in younger children and improves with age [1,2].
A considerable portion of patients seen on an average day in a pediatric clinic are boys who have not undergone circumcision and have nonretracting foreskins. For many of these patients, surgical intervention is not warranted. Many simply have adherence of the foreskin to the glans or they are infants who are best treated expectantly. Circumcision and topical steroids are now options for boys with persistent phimosis. When parents discover that there is a cautious, nonsurgical method for treating phimosis, they are often happy.
Using betamethasone cream, Golubovic et al. reported a 95% success rate in treating 20 boys [3]. Wright reported an 80% success rate after using betamethasone to treat 111 patients [4]. Some have reported success when using various topical medications. Strong corticosteroid clobetasol propionate has been shown to have success rates of 67 and 70%, respectively, according to Lindhagen [5], Jorgensen, and Svensson [6]. With a 75% success rate, Atilla et al. reported treating phimosis with a nonsteroidal anti-inflammatory ointment [7]. Our 90% success rate is in line with earlier reports.
Mechanism of topical steroid: Topical steroids have effects on skin thinning, immunosuppression, and anti-inflammatory properties [8]. When treating phimosis, the steroid may thin, increase the elasticity of the foreskin, and lessen any inflammation. It enables daily hygiene and the retraction of the foreskin. The topical steroid's effect seemed to be significantly better than the placebo's in one of the two randomised controlled trials comparing the two [9]. Another trial's outcome was not statistically significant, which could have been caused by an inadequate sample size. The ointment containing 0.05% betamethasone dipropionate was categorized as a strong corticosteroid. According to a review by Hepburn et al. of the topical steroids' safety and efficacy, side effects are extremely uncommon [10]. We had reported no local side effects during our follow-up period.
Mechanism of boric acid powder: Boric acid's antibacterial (bacteriostatic) and antifungal qualities make it an effective antiseptic [11]. This aids in the medical treatment of phimosis by treating bacterial and fungal infections that may be present on prepuce. In our study, we recommend that parents clean their prepuce with povidone iodine solution before fomenting it with two pinches of boric powder in 100 millilitres of lukewarm water.
Mechanism of povidone iodine solution: Povidone-iodine exhibits a wide spectrum of antimicrobial activity against viruses, bacteria, fungi, and protozoa. Its mode of action involves delivering and penetrating iodine to the surface of the pathogen cell. Key proteins, nucleotides, and fatty acids in the cytoplasm and cytoplasmic membrane are oxidized by iodine, which inactivates the molecules necessary for survival and results in cell death in a matter of seconds12. We applied a 5% povidone iodine solution to the prepuce following a mild retraction.
Conclusion
In particular, when applied in conjunction with the application of povidone iodine solution and boric powder fomentation, topical steroids prove to be a safe and effective treatment for phimosis. When considering circumcision, a trial of this medical treatment ought to be made available, and parents should be given adequate information before deciding whether to manage their child's phimosis surgically or medically.
References
- Gairdner D. The fate of the foreskin. A study of circumcision. Brit. Med. J., 1949; 2: 1433.
- Afr J Paediatr Surg, 2022; 19(4): 199–202. doi: 10.4103/ajps.ajps_143_21.
- Golubovic Z, Milanovic D, Vukadinovic V, Rakic I, Perovic S. The conservative treatment of phimosis in boys. Brit. J. Urol., 1996; 78: 786.
- Wright JE. The treatment of childhood phimosis with topical steroid. Aust. New Zeal. J. Surg., 1994; 64: 327.
- Lindhagen T. Topical clobetasol propionate compared with placebo in the treatment of unretractable foreskin. Eur. J. Surg., 1996; 162: 969.
- Jorgensen ET, Svensson A. The treatment of phimosis in boys with a potent topical steroid (clobetasol propionate) cream. Acta Dermato-Venereol, 1993; 73: 55.
- Atilla MK, Dundaroz R, Odabas O, Oztur H, Akin R, Gokcay E. A nonsurgical approach to the treatment of phimosis: local nonsteroidal anti-inflammatory ointment application. J. Urol, 1997; 158: 196.
- Dewan PA, Tieu HC, Chieng BS. Phimosis: is circumcision necessary? J. Paediatr. Child Health, 1996; 32: 285-289.
- Golubovic Z, Milanovic D, Viladompvoc V, Rakic I, Perovic S. The conservative treatment of phimosis in boys. Br. J. Urol, 1996; 78: 786–788.
- Hepburn DJ, Aeling JL, Weston WL. A reappraisal of topical steroid potency. Pediatr. Dermatol, 1996; 13: 239–245.
- Sobel JD, Sobel R. "Current and emerging pharmacotherapy for recurrent bacterial vaginosis". Expert Opin Pharmacother, 2021; 22(12): 1593–1600. doi: 10.1080/14656566.2021.1904890.
- Lepelletier D, Maillard JY, Pozzetto B, Simon A. Povidone Iodine: Properties, Mechanisms of Action, and Role in Infection Control and Staphylococcus aureusDecolonization. Antimicrob Agents Chemother, 2020; 64(9): e00682-20. doi: 10.1128/AAC.00682-20.

