Portal Venous Pseudoaneurysm a Rare Consequence of Blunt Abdominal Trauma
Rachida Chehrastane*, Sanae Jellal, Salma Marrakchi, Ihssan Hadj Hssain, Fatima Zahra Laamrani and Jroundi Laila
Emergency Radiology Department, Hospital Ibn Sina- Mohammed V University Rabat, Morocco
Received Date: 22/06/2024; Published Date: 08/10/2024
*Corresponding author: Rachida Chehrastane, Emergency Radiology Department, Hospital Ibn Sina- Mohammed V University Rabat, Morocco
Abstract
Vascular complications such as liver rupture and hepatic artery aneurysms and pseudoaneurysms are common after closed abdominal injury, especially blunt trauma, aneurysms and pseudoaneurysms of the portal system are rare but may also occur. Doppler US and multiplanar CT reconstruction can help confirm the diagnosis. The treatment depends on the clinical situation, although portal vein pseudoaneurysms can usually be treated conservatively. If complications occur or bleeding persists, transcatheter embolization or decompression surgery may be used.
Keywords: Portal pseudoaneurysm; Arteriovenous fistula; Blunt abdominal trauma; Angio CT scan; Doppler US
Case Report
We report the case of a 49 years old patient victim of a stab wound penetrating the right flank with a hemodynamic instability.
The abdominal CT scan identified a hepatic fracture involving segment IV and intraparenchymal hematomas of the segments IV and VIII, without an extravasation of contrast, conservative medical treatment was chosen, a control CT is performed one week later in front of the appearance of a diffuse abdominal pain, contracture of the right hypochondrium, diarrhea and hematemesis, how demonstrate abnormal communication between the right hepatic artery and the right portal vein associated to a giant pseudo aneurysm partially thrombosed of the right portal vein, with partial thrombosis of the portal trunk, and Esophageal varices splenorenal shunt, ascites, and liquefaction of intraparenchymal hematomas.
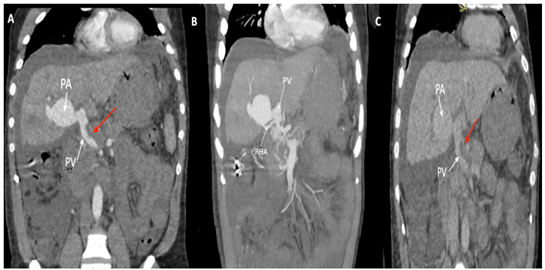
Figure 1: Sequential post-contrast coronal CT images of arterial phase (A) and (B: with maximum intensity projection MIP), image of portal phase CT (C), shows a large lobulated contrast-filled outpouching (PA) arising from the right branch of the portal vein (PV), and communicating with the right hepatic artery (RHA) suggestive of hepatic artery pseudoaneurysm with arterioportal fistula.
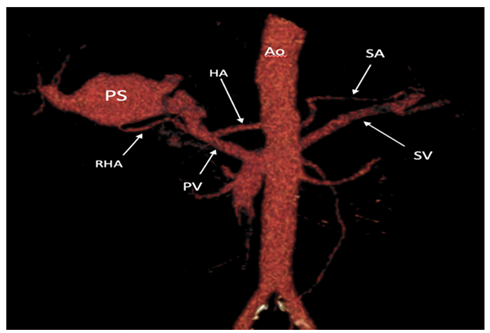
Figure 2: Three-dimensional reconstruction post contrast CT image demonstrate a voluminous pseudo-anerysm arising from a right branch of the portal vein, communicating with the right hepatic artery.PS (pseudoaneurysm), RHA (right hepatic artery), HA (hepatic artery), PV (portal vein), SA and SV (artery and splenic venal), Ao (abdominal aorta).
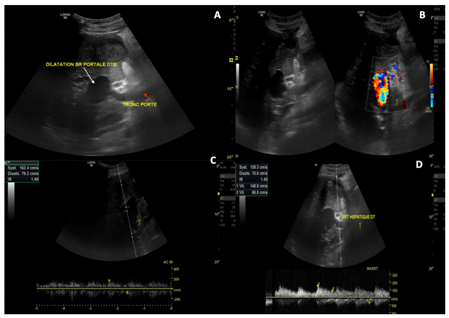
Figure 3: doppler ultrasound examination showed a pseudoaneurysm arsing the right hepatic vein (A,B) with an arterialization of the waveform of the downstream of the pseudoaneurysm (C), and increased systolic arterial flow and the index of resistancy of the right hepatic artery (D) ( systole 158 cm/s and IR: 1.45).
Discussion
Post-traumatic fistula may remain asymptomatic or cause abdominal pain and other severe symptoms caused by prehepatic portal hypertension such gastrointestinal bleeding or ascites, symptoms may appear over a variable period of 6 months to 5 years [1,2], they can be complicated by arterial pseudoaneurysms in 1.2% of cases [3,4] and more rarely by portal pseudoaneurysms how represent less than 0.4% [5,6].
The venous pseudoaneurysm are not defined as a focal dilation of a blood vessel, but a pulsatile hematoma that occurs when blood leaks from a fistula or rupture in the vessel wall or from blood trapped in surrounding parenchyma, the most common site is the main portal vein and branch sites of the intrahepatic portal vein, although extrahepatic portal vein aneurysms have also been reported [7].
Their evolution is characterized by an increase in size with a risk of portal system thrombosis, portal hypertension, and aneurysm rupture of in the bile duct, portal system, jejunum or peritoneal cavity.
However, in the absence of complications, these pseudo aneurysms remain asymptomatic, and are discovered either at the time of the appearance of clinical signs such hepatic colic, jaundice and hemobilia, [8] or during the monitoring CT scan [9].
Doppler ultrasound can be performed as a first-line examination, show a high-velocity connection between the artery and the portal vein, an arterialization of the vein downstream from the fistula, a simple dilatation of the downstream vein due to the increased volume of flow, and also the pseudoaneurysm, other signs may be found in case of complications, such as portal trunk thrombosis, collateral venous ciculations and ascite [10].
Abdominal CT with contrast, particularly the arterial phase of imaging, plays an essential role in the confident diagnosis of the condition. This is due to its multi-planar reformation, maximum intensity projection and 3D volume rendering capabilities, which allow better visualisation of fistulas by early attenation of the vein in arterial phase, as well as the identification and characterization of pseudoaneurysms.
It may also present with associated manifestations such as esophageal and gastric varices, diffuse gastrointestinal bleeding, ascite, and other arteriovenous malformations such as pseudoaneurysm [11].
Treatment depends on clinical manifestations [12], monitor asymptomatic patients without associated hepatic abnormalities or portal hypertension, doppler ultrasound is particularly useful for this monitoring.
If the aneurysm enlarges or complications develop, decompression surgery can avoid the progression of the aneurysm expansion [13]. The portal venous system is a low-pressure system, so conservative treatment is usually successful. However, if bleeding persists, catheter embolization can be performed using selective portography [14].
Conclusion
Vascular complications such as liver rupture, hepatic aneurysms, and pseudoaneurysms commonly occur after blunt abdominal trauma. Although less common, aneurysms and pseudoaneurysms of the portal venous system may also occur. Multiplanar CT reconstruction plays a crucial role in confirming the diagnosis, and treatment strategies vary depending on the clinical presentation. Portal vein pseudoaneurysms are usually amenable to conservative treatment, whereas transcatheter embolization may be required in cases of complications or ongoing bleeding.
References
- Fabian TC, Croce MA, Stanford GG, et al. Factors affecting morbidity following hepatic trauma. A prospective analysis of 482 injuries. Ann Surg, 1991; 213: 540-547.
- Numan C, Richard C, Semelek A, Jeet S, Sandhu A. Intrahepatic arterioportal fistula: gadolinium-enhanced 3D arm findings and angiographic embolization with steel coils. Magn Reson Imaging, 1999; 17(3): 475-478.
- Umut Oguslu, Sadik Ahmet Uyanik, Burçak Gümüş Endovascular treatment of hepatic arterioportal fistula complicated with giant portal vein aneurysm via percutaneous transhepatic US guided hepatic artery access CVIR Endovascular, 2019; 2: 39.
- Marcheix B, Dambrin C, Cron C, et al. Embolisation transhépatique percutannée d’un pseudoanevrysme posttraumatique de l’artère hépatique. Ann chir, 2004; 129: 603-606.
- Sarsilmaz A, Apaydin M, Yetkin U, Oziz E, Varer M, Yurekli I, et al. Portal vein aneurysm due to traumatic etiology. Int Journ Thorac Cardiovasc Surg, 2009; 13: 1.
- Koc Z, Oguzkurt L, Ulusan S. Portal venous system aneurysms: imaging, clinical findings, and a possible new etiologic factor. Am J Roentgenol, 2007; 189(5): 1023–1030.
- Blasbalg R, Yamada RM, Tiferes DA. Extrahepatic portal vein aneuryms. Am J Roentgen, 2000; 174: 877.
- Regent D, Laurent V, Meyer-Bisch L, Barbary-Lefèvre C, Corby-Ciprien S, Mathias J. La douleur biliaire : comment la reconnaître ? Comment l’explorer ? J Radiol, 2006; 87: 413-429.
- Becker CD, Mentha 9 G, Terrier F. Blunt abdominal trauma in adults: role of CT in diagnosis and management of visceral injuries. Eur Radiol, 1998; 8: 553-562.
- Bolognesi M, Sacerdoti D, Bombonato G, et al. Arterioportal fistulas in patients with liver cirrhosis: usefulness of color Doppler US for screening. Radiology, 2000; 216: 738–743.
- Choi BI, Lee KH, Han JK, et al. Hepatic arterioportal shunts: dynamic CT and MR features. Korean J Radiol, 2002; 3: 1–5.
- Feliciano PD, Cullen JJ, Corson JD. The management of extrahepatic portal vein aneurysm: observe or treat? HPB Surgery, 1996; 10: 113–116.
- Lau H, Chew DK, Belkin M. Extrahepatic portal vein aneurysm: a case report and review of the literature. Cardiovasc Surg, 2002; 10: 58–61.
- Laopaiboon V, Aphinives C, Pugkem A, Thummaroj J, Puttharak W, Soommart Y. Selective Transcatheter Embolisation for Treatment of Post-Traumatic Hepatic Artery and Portal Vein Pseudoaneurysms. J Med Assoc Thai, 2006; 89(2): 248–252.

