A Case of Acute Limb Ischemia Simultaneously Over Upper and Lower Limbs Successfully Treated by Rotarex Mechanical Thrombectomy
Po-Han Lee1,2, Nai-Yu Chi1,2, Ching-Tang Chang1,2, Tzu-Chieh Lin1,2, Tsung-Han Lin1,2, Tsung-Hsien Lin1,2,3 and Po-Chao Hsu1,2,3,*
1Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
2Division of Cardiology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
3Department of Internal Medicine, Faculty of Medicine, School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
Received Date: 13/06/2024; Published Date: 04/10/2024
*Corresponding author: Dr. Po-Chao Hsu, Division of Cardiology, Department of Internal Medicine; Kaohsiung Medical University Hospital, 100 Tzyou 1st Road, Kaohsiung. 80708, Taiwan, ROC
Abstract
Acute Limb Ischemia (ALI), constitutes a clinical emergency with the potential for limb loss and life-threatening consequences. Timely and precise diagnosis, as well as urgent intervention, are critical to preventing major complications such as limb loss and reperfusion syndrome. Herin, we presented a 69-year-old patient who suffered from simultaneously ALI at right lower and left upper limb and successfully treated with Rotarex thrombectomy. The patient with a history of atrial fibrillation and right hypopharyngeal cancer suffered from sudden onset of left arm and right lower limb pain, paresthesia, and persistent cold sensation. Emergent computed tomography scan confirmed left brachial artery thrombosis. Angiography revealed extensive thrombosis at the left brachial, ulnar, and radial arteries. A similar thrombotic picture was observed in the right external iliac artery and right femoral artery. We used Rotarex mechanical thrombectomy for both bilateral upper and lower limb thrombosis followed by catheter-directed thrombolysis. Follow-up angiography showed significant improvement of blood flow over both sites. The patient was discharged on Dabigatran without complications. This case demonstrates the efficacy of Rotarex mechanical thrombectomy treating simultaneous acute upper and lower limb thrombosis.
Keywords: Acute limb Ischemia; Rotarex Mechanical Thrombectomy; Catheter-Directed Thrombolysis; Acute upper and lower limbs Thrombosis
Introduction
Acute Limb Ischemia (ALI), characterized by a sudden decrease in limb perfusion within 14 days, constitutes a clinical emergency with the potential for limb loss and life-threatening consequences. Timely and precise diagnosis, as well as urgent intervention, are critical to preventing major complications such as limb loss and reperfusion syndrome [1]. In addition, simultaneous ALI over upper limb and lower limb are rarely reported in the literature. Herin, we presented a 69-year-old patient who suffered from simultaneously ALI at right lower and left upper limb and successfully treated with Rotarex thrombectomy.
Case Presentation
Our case was a 69-year-old male patient with multiple underlying medical conditions, including atrial fibrillation on long-term edoxaban therapy, concurrent right hypopharyngeal cancer with lung metastasis receiving chemotherapy, chronic kidney disease, and coronary artery disease. The patient was sent to our emergency department with sudden onset left arm and right lower limb pain, paresthesia, and persistent cold sensation. He had recently undergone right upper lobe lung wedge resection and had discontinued edoxaban therapy for 2 weeks.
Physical examination revealed a pale left upper limb and right lower limb with weak radial and dorsalis pedis pulsation. Laboratory tests indicated elevated levels of C-reactive protein at 43 mg/L and D-dimer at 9.04 mg/L. Electrocardiography demonstrate atrial fibrillation. Emergent left upper limb computed tomography angiography revealed thrombosis below the left brachial artery, confirming acute limb ischemia (Figure 1). Percutaneous angioplasty was immediately performed. Initial angiography revealed extensive thrombosis at the left brachial, ulnar, and radial arteries (Figure 2A). A similar thrombotic picture was observed in the right common iliac artery, right external and internal iliac arteries, and right femoral artery (Figure 3A). Fortunately, the bilateral renal arteries and superior mesenteric artery remained patent. After discussing with patient and family, Rotarex device was used for thrombosis over multiple arterial territories. After several times of thrombus suction, we successfully treated the patient with Rotarex thrombectomy over left brachial artery, and further performed angioplasty over ulnar, and radial arteries. Similar procedures were performed over the right external iliac and common femoral arteries. Fountain catheter were then placed in the left axillary artery and right common iliac artery for further Catheter-Directed Thrombolysis (CDT). Second angiography after 1-day CDT confirmed patent left brachial, ulnar arteries (Figure 2B), and right external iliac and common femoral arteries (Figure 3B). A follow-up brachial-ankle index assessment conducted two days later showed normal results, confirming the restoration of blood flow. The patient was discharged one week later, receiving long-term anticoagulation therapy with dabigatran without notable complications.
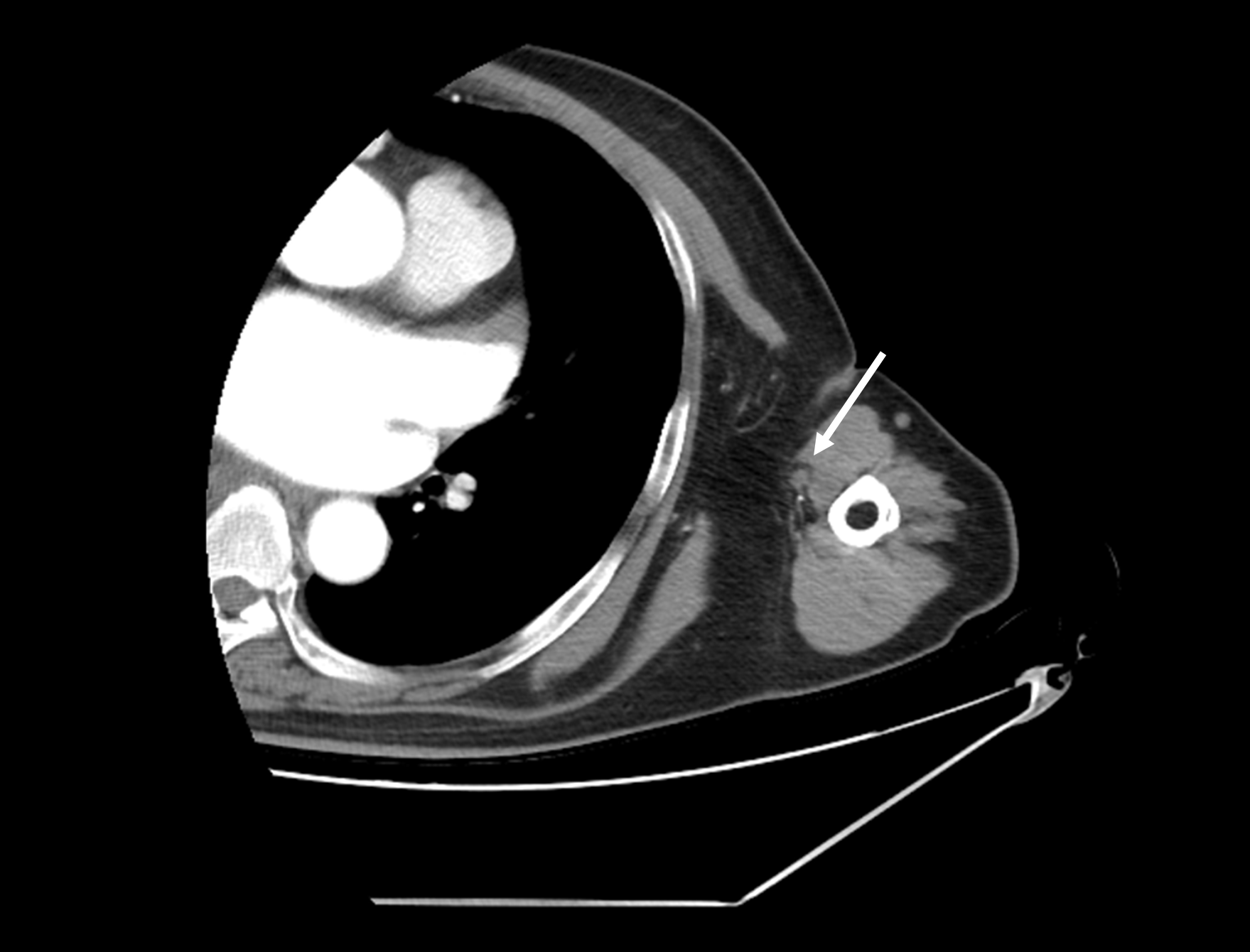
Figure 1. Left upper limb computed tomography with contrast demonstrating thrombosis (white arrow) at left proximal brachial artery.
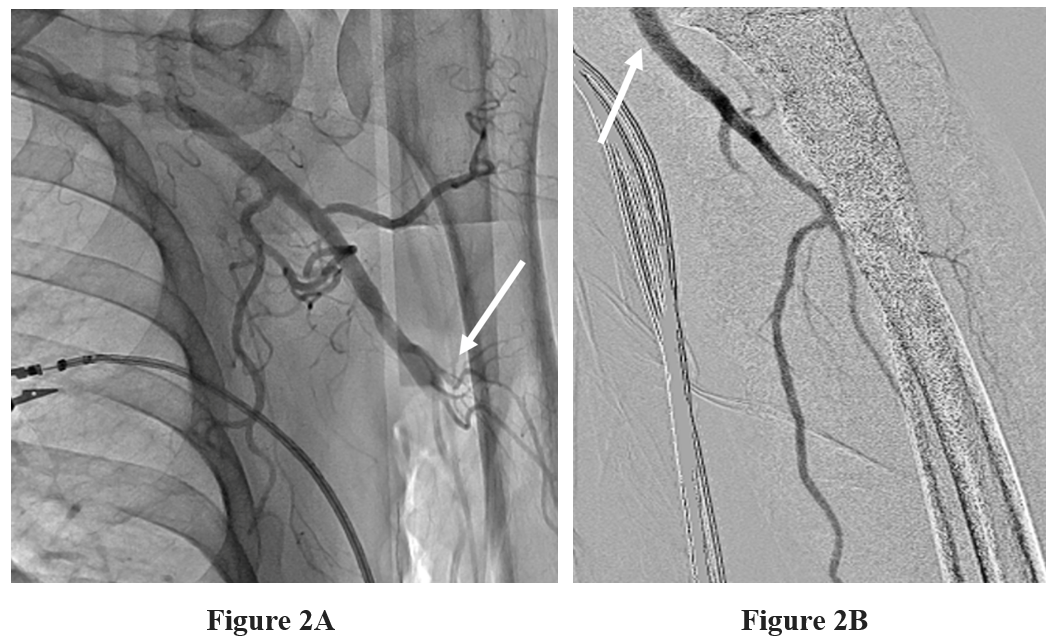
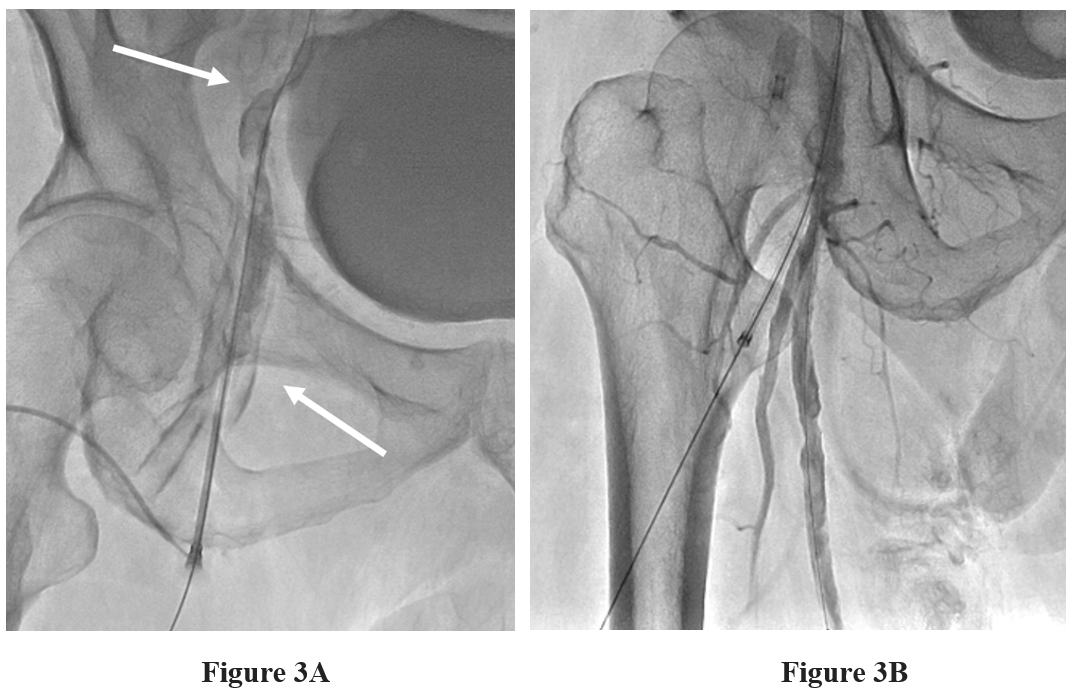
Figure 3: Angiography findings.
Figure 3A: Thrombus at right external iliac, and right femoral artery causing distal blood flow total occlusion (white arrow)
Figure 3B: Patent blood flow over right iliac artery, right common femoral artery, and right superficial femoral artery after Rotarex thrombectomy and CDT.
Discussion
ALI is a critical medical condition characterized by a sudden reduction in limb perfusion, carrying significant morbidity and mortality risks. With 30-day mortality rates ranging from 15% to 25% and a potential for 10% to 15% major amputation, urgent intervention is imperative to improve patient outcomes. Various treatment modalities have been employed, including anticoagulation, endovascular techniques such as aspiration, angioplasty, and stenting, catheter-directed thrombolysis, and surgical revascularization [1].
In recent years, the development of novel mechanical thrombectomy devices has revolutionized the field by enabling minimally invasive yet rapid removal of a substantial thrombotic burden within a short time frame. One such device, the Rotarex Device, operates on the principle of a spiral rotating at approximately 40,000 revolutions per minute, attached to the catheter's tip. This rotation induces thrombus fragmentation, facilitating subsequent aspiration-based thrombus extraction.[2] Rotarex have two different size options, 6F and 8F, targeting different vessel. 6F Rotarex device was recommended for 4-6 mm vessel diameter, and 8F aimed for vessel diameter greater than 6 mm. 6F Rotarex is favored for cases of acute ischemia over popliteal trifurcation and brachial artery, and the device of choice if follow-up thrombolysis is necessary for avoiding bleeding complication and inflow obstruction causing thrombus formation [3,4].
Notably, a study by Samuel Heller et al. in 2017 demonstrated the effectiveness of the Rotarex Device in reducing 30-day mortality rates, lowering amputation rates, and enhancing the success rate of revascularization in cases of ALI when compared to traditional thrombolysis. Furthermore, combining Rotarex and overnight fibrinolysis led to over 90% revascularization successful rate [4]. Building upon this foundation, our case presents a unique application of the Rotarex Device in a patient suffering from simultaneous acute upper and lower limb ischemia due to cardiac emboli. This intervention resulted in rapid restoration of blood flow and patient recovery without any notable complications.
Conclusion
To the best of our knowledge, this is the first documented case showcasing the efficacy of the Rotarex Device simultaneously treating ALI over lower and upper extremities. When considered alongside established treatment modalities, the combination of Rotarex thrombectomy with CDT emerges as a promising therapeutic option for the management of ALI.
References
- Current Treatment Options in Acute Limb Ischemia. Fortschr Röntgenstr, 2020; 192: 319–326.
- Percutaneous Mechanical Thrombectomy Using RotarexS Device in Acute Limb Ischemia in Infrainguinal Occlusions. Biomed Res Int, 2017; 2017: 2362769.
- Freitas B, Steiner S, Bausback Y, et al. Rotarex Mechanical Debulking in Acute and Subacute Arterial Lesions: Single-Center Experience With 525 Patients. Angiology, 2017; 68(3): 233-241.
- Retrograde rotational thrombectomy with the Rotarex® catheter system: treatment option for an acute thrombotic occlusion of a subclavian artery Vascular Health and Risk Management, 2011; 7: 623–627.

