Sturge Weber Syndrome in Adolescents
Paulino Insumbo*, El Mabrouk F, El Hamzi A, Rabileh Yassin M, Kessi E, Da Costa EBK, El Haddad S, Chat L and Allali N
Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Received Date: 09/03/2024; Published Date: 26/07/2024
*Corresponding author: Paulino Insumbo, Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University, Rabat, Morocco
Abstract
The word Sturge-Weber was given to Krabbe in 1934 in honor of two great men who contributed greatly to the study of this pathology (Willian Allen Sturge 1850-1919 and Frederick Parkes Weber 1863-1962), syndrome is a rare syndrome estimated at 1in 50000 live births [1,4], the diagnosis is always evoked at birth by detection of coloring in the supero-lateral part of the face of the newborn, which is called wine-bound, more image plays a very important role on all neurological manifestations, the reason for this work is that the vast majority of doctors usually act after the fist episode of epilepsy, which normally appears inthe fist years of life and in our case, only appeared in the tenth year, and the treatment will depend on the experience of doctors in particular neurology, ophthalmoogist and dermtologist.
Clinical Image
We present the case of a 13-year-old adolescent male patient, who was brought by his father to the emergency departmet of the children’s hospital in CHU de rabat in a state of epileptic disorder with no family history, physical or motor skills subsequently notable, absence of inbreeding history, but with, diagnosis at birth of a wine-colored flat angioma, affecting the upper part of the face on the right (Figure 1), physique examination, afebrile patient, with discreet eyelid ptosis a TDM was requested, which showing range of right fronto-parietal gyriform subcortical calcification, associated with calcification of the lenticular nuclei bilaterally and dilation of the right subepyndimal vein extended to the vein of galenia without minor hemorrhage with ipsilateral cortical atrophy (Figure 2), a week later an MRI was performed, actastic and tortuous apeearance of the superficial cortical veins bilaterally more marked on the right at the level of trolard and labbé veins draining at the level of the superior longitudinal sinus and the transverse sinus which are ectasia ; it is associated with multiple cortcal and juxta-cortical right hemispheric signal anomalies in T2 hyposignal and FLAIR, asinal the SWI sequences, producing a jellyfish heand appearance, enhanced in the vascular phase in relation to venous developmental anomalies ; hypertrophy of the choroid plexus with ectatic and tortuous ; and the patient appearance of the ependimary vascular structures and widening of bilateral cortical sulci calcium deposits were detected on the T2x sequence, thus the diagnosis of Sturge Weber syndrome was proposed, and the patient is on outpatient treatment.

Discussion
Sturge Webber syndrome is defined as a rare and sporadic congetital neurocutaneous and ocular phacomatosis that results from a malformation of the fetal vascular system leading to cortical anxiety in its complete form [1,5], Neurocutaneous syndrome observed in 1 in 50,000 individuals. According to Roach, Sturge Weber syndrome is classified into 3 types : type 1 combining facial angioma and leptomeningeal angioma with inconstant ocular involvement ; type 2 with facial angioma without involvement of the central nervous sytem and inconstant ocular involvement and type 3 with isolated leptomeningeal angioma, without skin involvement, and our patient is part of type 1 with is the more frequent classic form and the more severe prognosis. Sturge-Weber syndrome is not hereditary. It is caused by a somatic mutation (a change in DNA that occurs after conception at the level of precursors in the affected area) [2]. Sturge Weber Syndrome is characterized by the classic triad of a facial port-wine stain, leptomeningeal angiomatosis, and glaucoma [3]. Over the years, several authors and patholophysiologists have defined this syndrome as being distributed followinh-g the territory of the trigeminal nerve with a close relationship with this nerve, it was only after 2014 that a work team led by waelchli proposed that the distribution of this syndrome followed the territories of blood vessels, embrynic blood cells from the face and not from the trigeminal nerve. The fundamental physiopathological anomaly of facial capillary malformation is responsable for subcortical calcifications, the presence of abnormal vessels leads to an alteration of cerebral perfusion and an underlying condition which can worsen in the of uncontrolled convulsive seizures, [5]. Oculair abnormalities such as glaucoma and choroidal vascular disease associated with cortical atrophy present in most patients with this syndrome. Clinical manifestations of the syndrome include treatment-resistant epilepsy with hemianopsia and mental retardation. The diagnossis of Sturge Weber syndrome is suspected in patients presenting with a facial angiome after birth but CT and MRI without and with injection plai a very important rolefor the certainty and prognosis of patients with Sturge Weber syndrome.
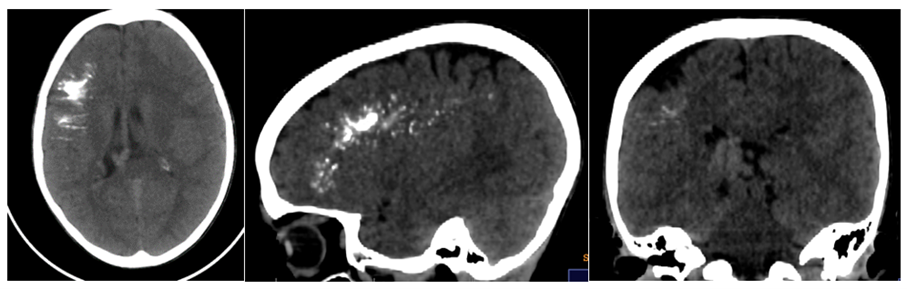
Image TDM
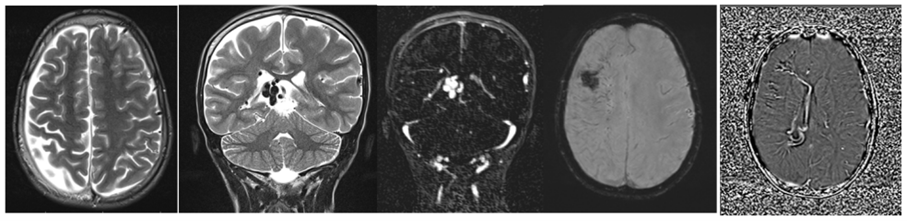
Images MRI
References
- Sturge-Weber syndrome: Optimization of the early diagnosis of pial angioma and search for electroencephalographic predictors of the development of epilepsy /Claire Bar Maillet Born on October 13, 1988 in Nantes November 15, 2017.
- Sturge-Weber syndrome, 2021.
- Bar Y Ainuz, Erin M Wolfe, S Anthony Wolfe. Surgical Management of Facial Port-Wine Stain in Sturge Weber Syndrome. Cureus, 2021; 13(1): e12637. doi: 10.7759/cureus.12637.
- Achint K Singh, Michael Keenaghan. Larousse Sturge-Weber-Krabbe's disease, or encephalotrigeminal angiomatosis.
- Meriem Doumiri, Mohamed Labied, Siham Salam, Dalal Laoudiyi, Kamilia Chbani, Lahcen Ouzidane. Sturge – Weber syndrome: A case report. Contemp Clin Dent, 2010 Jul-Sep; 1(3): 183–185. doi: 10.4103/0976-237X.72789.

