Seminoma on an Inguinal Ecopic Testis
Doumer A, Safwate R*, Al Afifi M, Moataz A, Dakir M, Debbagh A and Aboutaeib R
Departement of Urology, IBN Rochd University Hospital, Casablanca, Morocco
Received Date: 05/03/2024; Published Date: 15/07/2024
*Corresponding author: Safwate R, Departement of Urology, IBN Rochd University Hospital, Casablanca, Morocco
Abstract
Cryptorchidism stands as the most prevalent congenital malformation of the male genitourinary tract. An undescended testicle carries a 10% chance of developing cancer, with an intra-abdominal testicle posing the highest risk. In this report, we present the case of a 48-year-old fertile man who presented with a left inguinal mass persisting for 3 months. Upon scrotal examination, only one testis was found in the right scrotum, while the contralateral scrotum was empty, accompanied by swelling in the inguinal area. Subsequent radiologic examinations, followed by tumor excision and histopathological analysis, confirmed the diagnosis of a testicular seminoma. The patient was discharged without any complications and was subsequently referred to the oncology department for chemotherapy. Our findings reinforce the importance of early treatment and diligent monitoring of cases of cryptorchidism due to the associated risk of malignancy. Additionally, they underscore the necessity of conducting routine scrotal examinations in all males presenting with an inguinal mass.
Keyword : Cryptorchidism ; Inguinal testis ; Seminoma; Testicular
Introduction
Cryptorchidism refers to the condition where the testes fail to descend into the scrotum as expected during growth, instead remaining along their natural route of descent or in an abnormal location [1]. Seminoma represents the most common solid cancer in adult males aged 15 to 35 years old, with a higher propensity to occur in patients with cryptorchidism [2]. We report a case of a 48 years old fertile male, presenting an inguinal swelling for 3 months with the absence of the homolateral testicle. The patient underwent radical orchidectomy and was found caring a seminoma. Our findings underscore the importance of early treatment and vigilant monitoring of cases of cryptorchidism due to the associated risk of malignancy. Additionally, they emphasize the necessity of routine scrotal examinations in all males presenting with an abdominal or inguinal mass.
Case Report
We report the case of a 48-year-old patient, father of 3, who consulted the urology department of CHU Ibn Rochd, with no previous medical history, and who reported the appearance of a nonreducible and painless left inguinal swelling for 3 months (Figure 1). In addition, he reported a notion of left cryptorchidism since childhood, for which he had not consulted a doctor, given his low socio-economic status and rural origin.
Clinical examination confirmed the presence of a mass mobile in the superficial and deep planes, with no left testicle in the scrotum. The lymph nodes were free, the right testicle was normal and general condition was good. A testicular tumour was suspected.
An ultrasound scan was performed, which confirmed the presence of a vascularized tissue formation of the left testicle, which was in an inguinal position. The paraclinical work-up was completed by a thoraco-abdomino-pelvic CT scan and serum tumour marker quantification. The CT scan revealed an enlarged left testicle measuring 9x9.5 cm in an inguinal position, with no other secondary locations and no retroperitoneal adenopathy (Figure 2). Alpha-Fetoprotein (AFP) and Lactate Dehydrogenase (LDH) levels were normal, while Human Chorionic Gonadotrophin (HCG) was elevated at 24.08 mUI/mL.
Given these conditions, the patient underwent a left inguinal orchiectomy (Figure 3). An anathomopathological study of the specimen showed that the spermatic cord was resected over 4 cm and does not appear infiltrated on section. The testicle was covered by the albuginea, which was smooth and intact, with no signs of effraction. The tumour proliferation consisted of sheets of round cells, forming vague nodules, with large cells with eosinophilic cytoplasm and nuclei with heterogeneous granular chromatin. The stroma was lymphocytic, with a few granulomas. The tumor infiltrated the rete testis, while the epididymis, cord and hilar fat were unaffected. Search for vascular emboli was negative. Which concludes to an aspect of a pure seminoma (Figure 4).
The postoperative course was unremarkable and the patient was discharged from hospital. He was referred to oncology for adjuvant treatment.

Figure 1: Image showing left inguinal swelling.
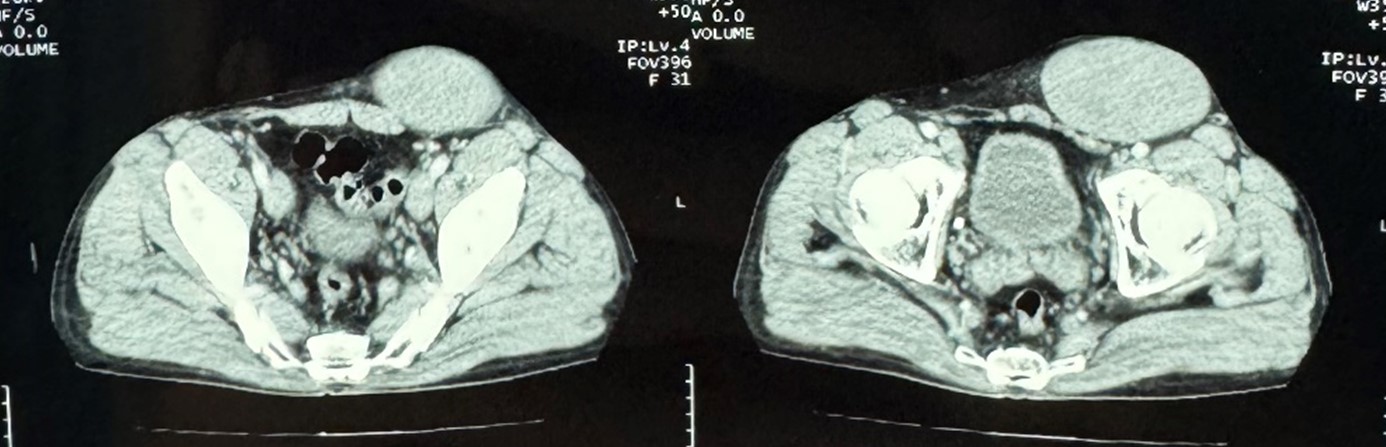
Figure 2: CT scan image showing the inguinal tissular mass.

Figure 3: Intraoperative image during inguinal orchiectomy.
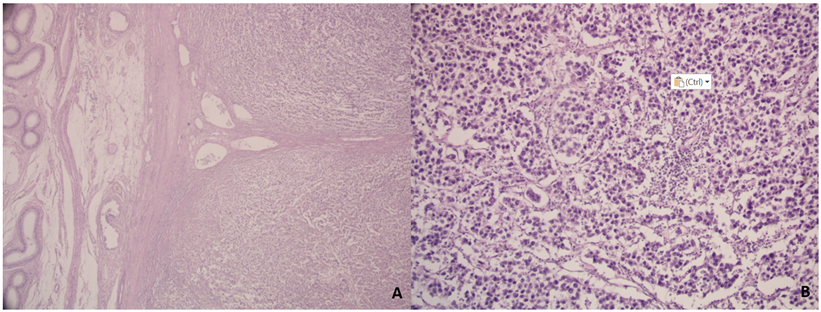
Figure 4: Histopathological study image. A : low enlargement: epididymis on the left and tumor on the right. B : Medium (20x) enlargement: round tumor cells in loosely lobulated clusters on a lymphocytic stroma.
Discussion
Cryptorchidism, the condition characterized by the absence of one or both testes from the scrotum, is the most prevalent birth defect of the male genitalia. It affects approximately 3% of full-term male neonates and up to 30% of preterm neonates. However, its occurrence decreases to 1% between the ages of 6 months and 1 year [1].
Several factors have been identified as predisposing to cryptorchidism, including prematurity, low birth weight, low gestational age, twinning, and maternal exposure to cigarette smoking and alcohol during pregnancy [1]. If left uncorrected between the ages of 6 months and 1 year, spontaneous descent of the testes is less likely to occur [3].
Cryptorchidism poses risks such as testicular cancer, ischemia, and infertility later in adulthood. Testicular seminoma is the most commonly observed malignant transformation of the undescended testis [4].
Testicular seminoma is a type of germinal cell tumor originating in the germinal epithelium of the seminiferous tubules within the testicle [2]. It accounts for approximately half of all testicular germ cell tumors and stands as the most prevalent malignancy among males aged 15 to 35 years [5]. Individuals with a prior history of cryptorchidism face a significantly heightened risk, being 10 to 40 times more prone to developing testicular seminomas [1].
The documented susceptibility of the undescended testis to malignant transformation, typically into seminoma, is widely acknowledged. This risk is notably reduced to 2 to 3 times the risk of the orthotopic testis if prepubertal orchidopexy is performed. Rates of malignancy in intra-abdominal testes have been reported as 5 times higher than the average malignancy rate in all undescended testes [6].
The undescended testis can be found at various points along the pathway of testicular descent, but the majority, around 66%, are situated distally to the external inguinal ring. Approximately 16% are located within the inguinal canal, while 10% remain in the abdominal region [7]. Additionally, it's noteworthy that an abdominal testis is four times more prone to developing tumors compared to an inguinal testis [8].
The exact pathophysiology driving the heightened risk remains unclear. Hypotheses suggest potential mechanisms such as abnormal temperature elevation leading to cell mutation, or the disruption of a shared regulatory pathway contributing to both maldescent and testicular cancer [9].
In cases of an undescended testicular seminoma, located in the abdominal area, clinical presentation can vary significantly. This range includes an asymptomatic mass to symptoms that mimic appendicitis, as well as symptoms related to mass effect or acute abdominal pain resulting from torsion or hemorrhage [7]. On the other hand, when it is located in the inguinal region, the most classic symptom is the appearance of a mass that mimics an inguinal hernia, but which is not reductible and can sometimes be painful, this highlights the importance of a scrotal examination in these situations [10].
Ultrasound exhibits a sensitivity as high as 95-97% in locating an inguinal testis. It could play a role in planning elective surgery to locate a non-palpable testis, as it may also detect a "peeping" testis, which is a testis that can variably be felt at the deep inguinal ring and can migrate back and forth through it. MRI may prove useful in identifying an intra-abdominal testis [10]. Seminoma typically manifests as a nodular appearance with homogeneous low signal intensity on T2-weighted MRI images [11].
The definitive diagnosis is ultimately established through histopathology. Histopathological examination typically reveals sheets of relatively uniform tumor cells with abundant clear or watery cytoplasm, characterized by large central nuclei with prominent nucleoli. These cells are often divided into poorly demarcated lobules by delicate fibrous septa and show minimal mitotic figures [2,5] The histopathological findings observed in our sample align with those commonly reported in the literature. If there is any doubt about the diagnosis, immunohistochemistry may be used. The tumour cells are positive for a panel of markers such as : SALL4, SDHB, CD117, D2-40, Ki-67 and PLAP [12].
Testicular seminoma can present and manifest itself through complications. The potential complications most frequently described in the literature are torsion of the cord of the tumor testicle and rupture of the testicle with hemorrhagic shock. (10) Abdominal cocoon syndrome has even been described, with a seminoma testis located intraabdominally [12].
Testicular cancer boasts a high survival rate of 97% at 5 years when detected and treated early [13]. However, delayed diagnosis can occur for various reasons, including patients not seeking medical advice regarding an otherwise asymptomatic empty scrotum or the challenge in diagnosing non-specific symptoms like abdominal ache or bloating [13,14]. Upon diagnosis, it's notable that 15% of pure seminomas have already metastasized and may present with symptoms such as abdominal pain or masses [14].
Initially, surgical management for adults with an uncomplicated intra-abdominal or inguinal testis typically involve orchidectomy, although there's been a shift towards conservative management with imaging surveillance. For patients with orthotopic testicular seminomas, approximately 80% of whom present with stage I disease, radical inguinal orchidectomy remains the preferred initial treatment. In the absence of adjuvant therapy, modern surveillance programs have shown a relapse rate of approximately 12–15% within the first three to four years, with an overall relapse rate of approximately 18%–20% over ten years [15].
Seminoma exhibits high sensitivity to radiotherapy and chemotherapy, and patients with stage I disease typically have favorable outcomes, achieving a 5-year cause-specific survival of 99.9% when treated with adjuvant chemotherapy and 100% when treated with adjuvant radiotherapy. More advanced disease may necessitate combination chemotherapy and radiotherapy, while lymph node dissection plays a more limited role due to a low rate of viable tumor in small residual masses and increased desmoplastic reaction and fibrosis following surgery [3,6,15].
In the presented case, no lymphadenopathy or other evidence of metastatic disease was observed. Consequently, the patient was referred for treatment with adjuvant chemotherapy.
Peer-reviewed guidelines advocate for orchidectomy in post-pubertal males with cryptorchidism as a means to minimize the risk of cancer [16,17]. Surveillance is only recommended for older patients who carry a significant anesthetic risk [16]. Beyond the malignancy risk, undescended testes do not seem to heighten the risk of fertility issues or testicular torsion [6].
Conclusion
This case underscores the importance of conducting testicular examinations when males present with abdominal symptoms or inguinal masses, as pain in these scenarios is often linked with testicular torsion and epididymo-orchitis. Additionally, it highlights the adverse outcomes associated with undescended testes and the potential advantages of early orchidopexy in reducing the risk of complications and facilitating future self-examination for testicular cancer. While guidelines and recommendations may vary among countries, most, including those from the American Urological Association, advocate for early orchidopexy. Pediatric surgical consultation should be sought if the testes have not descended by 6 months of age.
Conflicts of interest : The authors declare no conflicts of interest.
References
- Wood HM, Elder JS. Cryptorchidism and Testicular Cancer: Separating Fact From Fiction. J Urol, 2009; 181: 452–461.
- Rosai J, Louis S, Mills S, et al. Sternberg’s Diagnostic Surgical Pathology Advances in Anatomic Pathology, 2004; 11: 323–324.
- Cryptorchidism Treatment & Management: Medical Therapy Surgical Therapy, Preoperative Details.
- Cortes D, Thorup J, Petersen BL. Testicular neoplasia in undescended testes of cryptorchid boys-does surgical strategy have an impact on the risk of invasive testicular neoplasia? Turk J Pediatr, 2004; 46: 35–42.
- Rosai J, Louis S, Mills S, et al. Sternberg’s Diagnostic Surgical Pathology. Advances in Anatomic Pathology, 2004; 11: 323–324.
- Ashley RA, Barthold JS, Kolon TF. Cryptorchidism: pathogenesis, diagnosis, treatment and prognosis. Urol Clin North Am, 2010; 37(2): 183-193.
- Lim YJ, Jeong MJ, Bae BN, et al. Seminoma in undescended testis. Abdom Imaging, 2008; 33: 241–243.
- Yılmaz A, Bayraktar B, Sagiroglu J, et al. Giant seminoma in an undescended testis presenting as an abdominal wall mass. J Surg Case Rep, 2011; 2011: 9.
- Ferguson L, Agoulnik AI. Testicular cancer and cryptorchidism. Front.Endocrinol. (Lausanne), 2013; 4: 32.
- Rourke E, Digman G, Gourley E, et al. BMJ Case Rep. doi: 10.1136/bcr-2017-222670.
- Adham WK, Raval BK, Uzquiano MC, Lemos LB. Best cases from the AFIP: bilateral testicular tumors: seminoma and mixed germ cell tumor. Radiographics, 2005; 25(3): 835-839.
- Jiang-Lai Zhou, Dong-Qin Liu, Jian-Xiang Lei, Shu-Feng Zhao. Asian Journal of Surgery. Abdominal cocoon syndrome with unilateral cryptorchidism and seminoma: A case report. doi: 10.1016/j.asjsur.2022.07.059.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J. Clin, 2016; 66: 7–30.
- Velez D, Zhao P, Mayer T, Singer E. Intra-abdominal seminoma found incidentally during trauma workup in a man with bilateral cryptorchidism.Urol. Ann, 2015; 7: 534–536.
- Alexander EJ, White IM, Horwich A. Update on management of seminoma. Indian J Urol, 2010; 26(1): 82-91.
- Kolon TF, Herndon CD, Baker LA, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J. Urol, 2014; 192: 337–345.
- Radmayr C. Management of undescended testes: European Association of Urology/European Society for Paediatric Urology guidelines. J. Pediatr. Urol, 2017; 13: 550.

