Krukenberg Tumor Case Report
Paulino I*, Chaimae E, Domitiano BNM, Kessi Eric MC, Madina Rabileh Y, PR ADDAD and El Mandour G
Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Received Date: 04/11/2023; Published Date: 15/04/2024
*Corresponding author: Paulino Insumbo, Department of radiology, Pediatric hospital, UHC IBN Sina Mohamed V University Rabat, Morocco
Abstract
PA, of the bulbe is extremely rare and a very gloomy prognosis are the most common benign brain tumour in children and adolescents. Represents about 30% of all posterior cerebral fosse. Clinical data accompanied by Magnetic Resonance Imaging (MRI) and scanner combined with an intravenous contrast agent is particularly suitable for visualizing pilocytic astrocytomas and differentiating them from surrounding healthy brain tissue but currently been introduced diagnostic based on morphology, immonohistochimistry and the presence of key genetic alterations [1]. The treatment is always surgical with resection may provide reasonable prolongation of surviva. This article is to show the circumscribed and rare forms of pilocytic astrocytomas located in the bulb
Keywords: Astrocytoma pilocytique centered on medulla oblongata
Clinical Image
Imaging techniques play a key role in the diagnosis of pilocytic astrocytomas. Magnetic Resonance Imaging (MRI) and scanner combined with an intravenous contrast agent is particularly suitable for visualizing pilocytic astrocytomas and differentiating them from surrounding healthy brain tissue. This is 5-year-old patient wilh a private history, who was brought to the radiology services of the pediatric hospital, by his family members, who presented two months ago with diplopia, headache, accompanied by vomiting, vertigo ataxic gait, etc, occulomotor paralysis.
Krukenberg tumors are ovarian lesions metastatic, bilateral in at least 2/3 of cases, and which find their origin in several places including the most common sites are the colon (16 to 32%), the breast (8 to 16%), stomach (7 to 22%), appendix (3 to 20%) and the pancreas (2 to 5%) [2,3].
Other sites have also been described, such as the gallbladder and bile ducts, small intestine, ampulla of Vater, the cervix, the bladder and the urachus. Sometimes we don't unable to determine the location of the tumor primitive as it can be small and remain for a long time silent [1]. This sarcomatoid component is often accompanied by luteinization of stromal cells, explaining the signs of virilization sometimes described in Literature. Are therefore excluded from this denomination the primary ovarian tumors, lymphomas and others blood line neoplasia, tumors of origin genital, etc., [3].
Pathogeny
There is still disagreement about the exact mechanism by which cancer cells in the stomach, appendix or colon metastasize to the ovaries; traditionally we thought that contamination occurred directly through the abdominal cavity, but some Researchers have recently suggested that this contamination may more likely be lymphatic (i.e. through the lymph nodes) or hematogenous (i.e. i.e. through the blood), since most of these tumors are found inside the ovaries. Proponents of this theory have noted that metastases do not occur never in the omentum or omentum (fatty plate hanging from the stomach) and that the cells Cancer cells are found inside the ovary but do not grow outward.
Although a Krukenberg tumor is most commonly a metastasis from cancer gastric (usually an adenocarcinoma), this is not always the case. Others have been reported tumors of the gastrointestinal area (including, importantly, colon cancer) that have caused Krukenberg tumors and the medical literature reports recent cases where Krukenberg tumors arise from tumors at the tip of the appendix.
Discussion
The increase in alkaline phosphatase and PTH with serum calcium and normal phosphate levels as well as low calciuria and severe hypovitaminosis D suggested the possibility of osteomalacia secondary to severe chronic vitamin D deficiency and in calcium. This hypothesis could however be ruled out on the basis of the absence of braking sufficient PTH following correction of vitamin D deficiency and calcium intake, a bone assessment not compatible with this hypothesis and an osteodensitometry objectifying BMD values higher than normal. Primary hyperparathyroidism has also been quickly excluded based on the absence of hypercalcemia and hypophosphatemia, frank hypocalciuria as well as supranormal BMD values.
The assessment carried out therefore indicates the presence of an extensive osteoblastic tumor process. Major activation of osteoblasts leads to intense calcium consumption circulating, thus causing a tendency to hypocalcemia. This stimulates the secretion of PTH which immediately compensates for the drop in calcium by digestive and renal reabsorption, which explains the normal serum calcium, the very low calciuria (all the calcium is directed towards bone), and increase in PTH.
Bone turnover is generally increased, with an increase in alkaline phosphatase bone and C-terminal telopeptides. This hypothesis is reinforced by scintigraphy bone and PET-CT which show numerous hypermetabolic bony foci, no lytic on standard radiographic examination.
The appearance of moderately hypermetabolic ovarian tumors, characterized as TK based on MRI, as well as peritoneal tumor nodules, confirms the presence of a metastatic tumor process. The formal diagnosis of poorly differentiated adenocarcinoma cells in rings at kitten was finally posed based on the histological analysis of the
bone and marrow biopsy, and that of TK based on histological analysis of the tumor left ovary.
Krukenberg tumors are metastatic ovarian lesions, bilateral in at least least 2/3 of cases, and which find their origin in several places including the most common sites common are the colon (16 to 32%), breast (8 to 16%), stomach (7 to 22%), appendix (3 to 20%) and the pancreas (2 to 5%) (2.3).
Other sites have also been described, such as the gallbladder and bile ducts, intestine small intestine, the ampulla of Vater, the cervix, the bladder and the urachus. Sometimes we fail to determine the location of the primary tumor as it may be small and remain silent for a long time. The entity of primitive TKs, for its part, remains controversial [1].
In the reported case, the major symptom of TK is the appearance of hypogastric pain. And lower lumbar, present in 42% of cases. More rarely, we can observe metrorrhagia (18%), increased abdominal circumference (15%) and weight loss (6%) [3]. The mode of presentation here is particular, due to the young age of the patient (29 years), the average onset of TK being 45 years (1.7), and on the other hand, due to the elevation significant increase in PTH levels and the presence of osteoblastic metastases. In the litterature, some cases of paraneoplastic PTH secretion have been described from various tumors of non-parathyroid origin [6]. However, this hypothesis could be excluded in the case reported. Other rare modes of presentation of TK have been described in the literature, such that virilization by production of hormones by the ovarian stroma, or even a pseudo-Meig syndrome, mimicking a benign ovarian mass with ascites and hydrothorax [8,9].
Since only 5-15% of ovarian tumors are of metastatic origin, it is essential to exclude a primary ovarian tumor. This is done on a biological basis, morphological and histological. MRI and ultrasound are both types of imaging
allowing the characterization of an ovarian tumor. According to one study [10], multilocularity is rather in favor of a primary ovarian tumor, with a positive predictive value of 91% on ultrasound and 89% on MRI, while the negative predictive values are 71 and 61% respectively.
On the other hand, although ovarian metastases are most often bilateral, the presence a mass in each ovary alone does not rule out an ovarian tumor primitive, since depending on its type, it can still present itself in both ovaries synchronously. Among the metastases, those of cancers of the stomach, breast and of the endometrium have a rather solid appearance, while those of the colon have a tendency cystic. In the case described, the morphology of the tumors argued for TK since, despite the multilocular appearance of the ovarian masses, these had appeared in a context metastatic.
According to the WHO, the formal diagnosis of TK is based on three conditions [11]: (a) invasion tumor stromal; (b) the presence of neoplastic ring-shaped cells producing mucin; (c) sarcomatoid ovarian stromal proliferation. This component sarcomatoid is often accompanied by luteinization of stromal cells, explaining the signs of virilization sometimes described in the literature. Are therefore excluded from this naming primary ovarian tumors, lymphomas and other neoplasias of the blood lines, tumors of genital origin, etc., [3].
On immunostaining, a primary ovarian tumor will most often have a CK7+/CK20- immunophenotype, but the same phenotype is found in metastases ovaries of an adenocarcinoma of mammary origin, upper gastrointestinal (stomach, small intestine, appendix), pancreatic or biliary, while colonic adenocarcinomas express almost always cytokeratin 20 [1,4,5]. Immunohistochemistry of bone biopsies and ovaries, only CK7 was positive. If we follow the reasoning proposed by Kriplani et al. [5], this therefore suggests an adenocarcinoma whose origin is either gastric, or mammary, or appendicular or even hail, these last two hypotheses being reinforced by the focus mesenteric objectified on PET-CT. Suspected based on wall thickening on MRI and of the presence of an ulcer, the gastric origin could not be confirmed by deep biopsies which showed no signs of malignancy. However, this does not exclude this hypothesis formally. The mammary origin was, however, ruled out on the basis of an assessment negative senological and the absence of marking for mammoglobin. The color origin rectal is much less likely based on immunohistochemical markers and rest of the assessment carried out, but it should be noted that a colonoscopy was not carried out. Finally, the Tumor markers CEA, CA19.9, CA15.3, hCG and α-feto-protein were all negative.
The original site therefore remains undetermined at this stage. The median survival of patients with TK is approximately 16 months with a rate of 80% death within two years. Poor prognostic factors are site discovery primary after the appearance of TK, TK of gastric origin or of undetermined origin, resection of the primary tumor at the same time or after resection of TK, the presence of metastases elsewhere than in the ovaries, the elevation of the CA125 level, the presence of ascites and pelvic invasion. TK size, bilaterality and age have no influence on mortality (1.12).
When the primary site is known and resected and there is no other metastatic site, we can obtain a considerable increase in survival by metastasectomy of TK and cytoreduction. In TK of undetermined origin, laparoscopy may also be performed to try to locate the primary tumor and perform an adnexectomy in order to relieve pain due to pelvic masses and perform a histological analysis of the ovarian tissues. At laparoscopy, TKs classically have a smooth macroscopic appearance, bumpy and without adhesions or peritoneal graft coming from these metastases, which gives a falsely benign appearance (1.12).
Wu et al. [12] showed, in a retrospective study of 128 patients with TK, that a chemotherapy in 4 to 6 cycles by combination of dual or triple therapy of platinum salts, 5-FU and taxanes also significantly extended survival with survival at 12 months of 80% with chemotherapy versus 40% without chemotherapy. In conclusion, we we report the exceptional case of a young patient with Krukenberg tumors bilateral multilocular appearance, of undetermined origin and atypical presentation with osteoblastic metastases, acceleration of bone turnover and elevation of PTH levels.
The definitive diagnosis was made by histological analysis of bone biopsies and ovarian. However, despite the techniques available to us to identify the origin of such tumors, such as imaging, biological markers and immunohistochemistry, we We were unable to locate the primary site of the condition. TKs of undetermined origin are poor prognosis since they are often discovered at an advanced stage with extension to other organs, as described in our situation.
The treatment consists of resecting the primary site and the annexes when the extension assessment does not shows no other metastatic site. Certain platinum salt chemotherapy regimens, 5-FU and/or taxanes have shown encouraging results regarding the short-term survival of patient, but less satisfactory in the long term. Multidisciplinary care global approach is therefore necessary in order to discuss the therapeutic project to be adapted according to tumor extension, prognostic factors and patient comorbidities.
Pilocytic Astrocytoma (PA) Amont the most common primary benign tumors, they are low-grade tumors according to the classification of the world cerebral tumor [4]. A PA develops from certain star-shaped brain cells called astrocytes. Astrocytes and similar cells form tissue that surrounds and protects other nerve cells found within the brain and spinal cord, tumor. Symptoms of a PA will vary depending upon the size and also of location of the tumor. Symptoms resulting from this pathologie we can mention increased pressure on the brain and include headaches, nausea, vomiting, balance problems and vision abnormalities [3,8]. The tumor is most often located in the cerebellar hemisphere, but in our case, it’s an expansive process of BCF, centered on the bulb, with dual tissue (Figure 2), component in hypersignal T2 and FLAIR, heterogeneously enhanced after injection of PC and a cystic component in hypersignal T2, hyposignal T1 and diffusion b 1000, intermediate signal in FLAIR, enhanced in the periphery after injection of PC. It is surrounded by a discrete perilesional edema in hypersignal T2 and FLAIR and exerts a mass effect on the lower part of the V4 which is collabée, as well as on the cerebellar tonsils, pushed back. It is responsible for an erasure of the peribulbar cisterns, with filling of the occipital hole. MRS shows a moderate reversal of the choline/NAA ratio, with the presence of inositol peaks and short-echo lactates. Absence of ventricular sus tentorial dilatation. Absence of intraparenchymal signal abnormalities in addition to tentorial. The centreline structures are in place.

Figure 1: axial(a), sagittal(b) and coronal(c); CT without injection, showing circumscribed lesional process centered on dual tissue and cystic medulla oblongata, with discrete repression of the 4th ventricle without evidence of hydrocephalus.
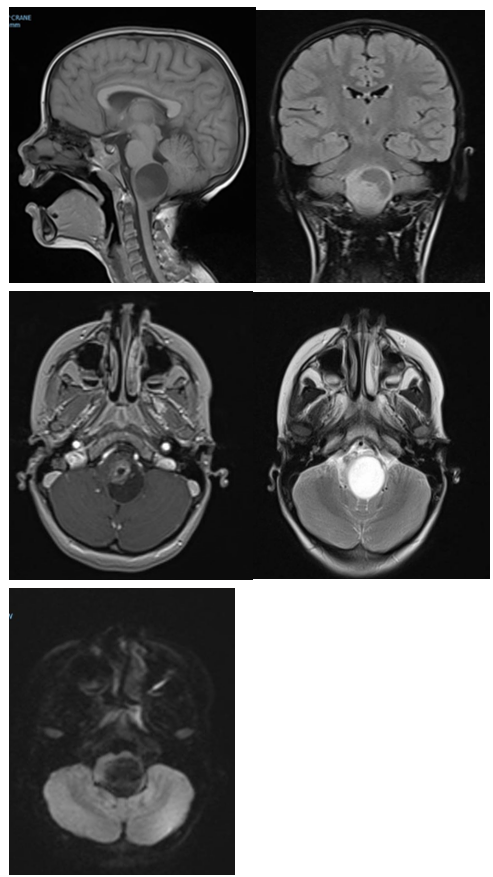
Figure 2: sagittal section (a) lesion centered on the bulb with dual tissue.
Practical recommendations
- The search for a primary site and other metastases is essential in any suspicion of Krukenberg tumor, because the therapeutic attitude and the vital prognosis depend on it. We will therefore carry out: gastroscopy, colonoscopy, echo-endoscopies, breast assessment, PET-CT, etc.
- If no origin is established and no other metastatic lesion has been identified, the Diagnosis will be made on the basis of a laparoscopic adnexectomy. It can be done by puncture biopsy in case of proven peritoneal/pelvic/... dissemination.
- When the primary site is known and there is no other metastasis than the lesions ovaries, it is advisable to carry out a resection of the primary site and the metastases, associated to chemotherapy. If there are other metastases, treatment will mainly consist of chemotherapy, but resection of the ovarian masses for analgesic purposes may also be considered.
References
- Alice Métais, andrey Rousseau: Histomolecular diagnosis of glial and glioneuronal tumors, Department of Cellular and Tissue Pathology, CHU Angers, 2 rue Larrey, 49100, Angers, France.
- Pilocytic Astrocytoma - Philippe Schucht, levin Hani
- Primary spinal pilocytic astrocytoma: clinical study with long-term fallow-up in 16 patients and a literature review.

