Diabetes and Mental Health in California Emergency Department Visits
Jim E Banta*, Mayur Rawal, Kushinga M Bvute, Gina Obiakor, Jessica Mosher and James M Banta
School of Public Health, Loma Linda University, USA
Received Date: 12/10/2023; Published Date: 21/03/2024
*Corresponding author: Jim E Banta, PhD, School of Public Health, Loma Linda University, 24951 North Circle Drive, Loma Linda, CA, 92350, USA
Abstract
Background: The purpose of this study was to examine prevalence of diabetes and mental illness diagnoses among California Emergency Room/Department visits.
Methods: Public-use data (2005- 2014) was obtained from the California Office of Statewide Health Planning and Development (OSHPD) for 357 community-based hospitals. International Classification of Diseases, Ninth Edition (ICD-9) diagnoses were used to identify diabetes mellitus (250.x) and mental illness/substance abuse via Clinical Classification Software categories. Graphs were generated for all visits, followed by bivariate and logistic regression of diabetes-related visits.
Results: There were 97,639,808 million ER visits between January 1, 2005 and December 31, 2014, of which 6,484,950 (6.64%) had any diabetes diagnosis. The number of diabetes-related ER visits increased from 342,106 in 2005 to 1,008,154 in 2014. Between 2005 and 2014 the percent of diabetes visits having a mental diagnosis increased from 10.1% to 19.5%, while a mental diagnosis increased from 7.7 to 13.3% among non-diabetes visits. Diabetes was primary diagnosis in 10.76% of diabetes visits. Non-routine discharge, mostly being hospitalized or transferred to another facility, occurred in 8.5% of primary-diagnosis visits and 8.1% of secondary-diagnosis visits. Predictors of non-routine discharge included a handful of mental diagnoses, notably suicide/self-harm (odds ratio OR 4.5), delirium/dementia (OR 3.67) and schizophrenia (OR 3.45), hospital being rural, and patient having private insurance.
Conclusion: Increases in ER visits having a diabetes diagnosis as well as increasing comorbid mental illness suggests need for improvements in primary care. Higher likelihoods of being treated-and-released among Medicaid and self-pay patients may reflect lower quality of outpatient care.
Keywords: Emergency service; Mental health; Diabetes mellitus; Prevalence; Comorbidity; Hospitals
Background
An estimated 34.2 million people have diabetes (10.5% of the US population), with 7.3 million (21.4%) of those likely having diabetes being undiagnosed [1]. The projected number of adults with diagnosed diabetes is projected to increase from 22.3 million (9.1% of population) in 2014 to 39.7 million (13.9%) in 2030, and to 60.6 million (17.9%) in 2060 [2]. Diabetes is also the seventh leading cause of death in the United States [3].
The American Diabetes Association estimated the total costs of diagnosed diabetes have risen from $245 billion in 2012 to $327 billion in 2017 [4]. Based on national health expenditure accounts, in 2013 it was determined that mental illness was the single most costly condition, with spending at $201 billion [5]. The NHEA approach is more conservative and does not include indirect costs. In 2013 expenditures for diabetes were estimated at $62 billion [5]. It is estimated that 1 in 5 U.S. adults experience mental illness each year, with mental illness and substance use disorders being involved in 1 out of every 8 emergency department visits by a U.S. adult – roughly 12 million visits [6].
The estimated annual number of emergency room visits in the United States has increased from 128,885,040 in 2009 to 143,454,430 in 2018 [7]. In 2015 it was estimated that 12 million ED visits were made by patients aged 45 and over with diabetes, accounting for roughly 25% of all ED visits by patients aged 45 and over [8]. The diabetes ED visit rate was about 6 times higher than the diabetes ED visit rate for those under age 45 [8]. Between 2009 and 2015 the rate of mental health-related ED visits increased by 56.4% for pediatric patients and 40.8% for adults, accounting for approximately 10% of ED visits and 11.1% of adult ED treatment hours [9].
The relationship between diabetes and mental illness may be bidirectional in nature, with each exacerbating the symptoms or playing an important role in the development of the other [10]. For example, diabetes-related complications increase functional impairment which in turn leads to greater depression [11]. Americans with Type II diabetes have a 25% chance of also being comorbid with depression [12] and individuals with schizophrenia have at least double the risk of developing diabetes [13]. People with diabetes have a higher risk of developing mental health disorders, particularly depression, anxiety, eating disorders and Serious Mental Illness (SMI) [14] and there is a higher risk of mental illness and suicide among young adults with diabetes [15].
Diabetes outcomes for people with SMI are also poorer as these patients experience a higher risk of and macrovascular complications [16]. Suspected mechanisms for higher mortality include genetics, environmental and disease-specific factors, and treatment-specific factors [17]. Comorbid mental illness and diabetes may interfere with adherence to treatment, complicating the abilities of providers to treat and manage comorbid illnesses. For example, analysis of Medical Expenditure Panel Surveys (MEPS) for the years 2010-2014 found that as many as 71% of those with schizophrenia were found to be nonadherent to antipsychotic medications [18]. Those having medical comorbidity had more emergency department and inpatient utilization compared to those without medical comorbidity [18]. Thus, patients with diabetes and co-occurring psychiatric disorders are more likely to have poor health care quality, poor glycemic levels, increased emergency room visits, and higher rates of hospitalization [19].
Given the increasing prevalence of both diabetes and mental illness in the United States, this study aims to (1) determine the prevalence of comorbid diabetes and mental illness among the population of people who visited the Emergency Room in the state of California over a ten-year period; (2) explore differences between those having diabetes as a primary or secondary diagnosis; and (3) identify factors associated with non-routine discharge of diabetes-related ER visits.
Methods
Data
Emergency Room (E.R.) visit public-use data were obtained from the California Office of Statewide Health Planning and Development (OSHPD) for community-based hospitals, excluding federal hospitals. There was one row of data for each of the 97,639,808 million ER visits between January 1, 2005 and December 31, 2014. Patient-level data obtained included year treated, expected source of payment, primary diagnosis, up to 24 secondary diagnoses, and disposition of discharge [20]. Through 2011 the public-use data had included patient gender, race, ethnicity, age category, and five-digit ZIP Code of residence. From 2012 to 2014 public-use data included only the five-digit ZIP Code of residence. Since the OSHPD data did not have reliable patient ZIP code data, area-based socio-demographic data at the hospital level were obtained. This included those in poverty and college graduates among adults 25 years of age and greater at the Congressional District level [21] and population density and percent non-Hispanic white at the Medical Service Study Area [22].
OSHPD provides hospital-level data via annual files which include information such as bed size in addition to hospital-level summary patient demographic data and geographic identifiers for each hospital, such as the city, ZIP Code, county, Congressional district, and Medical Service Study Area in which the hospital is located [23]. There were 357 hospitals that provided data during the study period.
Subjects
All ER visits were examined, with a focus on those having an International Classification of Diseases, Ninth Edition (ICD-9) diagnosis of any diabetes mellitus (250.x).
Measures
Mental illness was measured using the Clinical Classification Software (CCS) schema [24] developed by the Agency for Healthcare Research and Quality. CCS categorizes thousands of individual ICD-9 codes into 270 mutually exclusive and clinically meaningful categories schema [24]. All 25 diagnosis fields within the ER visit data were searched for diagnoses meeting the definition of the 14 CCS categories for mental illness and substance abuse. Hospital-level measures included bed size, academic affiliation, rural/urban status, and ownership type. Area-based measures included percent of population in poverty, college graduates among adults 25 years of age and greater, population density and percent non-Hispanic white. Patient-level measures included age group, gender, race and ethnicity. The primary outcome measure was non-routine discharge. This primarily includes hospitalization and transfer to another facility; but also includes leaving against medical advice and mortality.
Analysis
Analysis was guided by Andersen’s Behavioral Model of Health Services Utilization [25]. The conceptual model considers the effects of individual characteristics (predisposing, enabling, and need) on access to healthcare and also considers contextual effects, that is, factors related to the environment and health care system. Mental illness and substance abuse were considered as a personal predisposing – vulnerable domain measure [26].
A significant issue arose due to partially masked demographic data from 2005 to 2011 and completely missing demographic data from 2012 to 2014. A Markov Chain Monte Carlo method [27] was used to impute missing values of age, gender, race, and ethnicity, as has been done in other analyses involving public-use inpatient data [28,29]. Multiple imputations were done using known patient gender, age, race, and ethnicity data, and patient payer source. Also used in imputation were hospital-level summary measures such as the percent of discharges which were female, white, age less than 18 years, age greater than 60 years, and percent Spanish-speaking. ICD-9 codes were used to identify gender and age-specific visits, such as female, e.g., pregnancy-related codes accounted for 5% of all visits, male reproductive-related codes accounted for 1% of all visits, and newborn/infant-related for 0.2% of visits). Of the 97.6 million records, there was substantial masked/missing data for demographics: gender (37.75% missing data), age group (36.62%), race (45.94%), and ethnicity (48.26%). Because expectation-maximization works best with continuous measures, race was imputed as white/non-white rather than as multiple categories and age as greater/less than 45 years of age. All imputed demographic measures were used as a continuous variable ranging from 0 to 1.
The entire 97 million record dataset was used to examined trends. A figure was created to show the annual percentage of ER visits having a mental diagnosis, both for cases having a diabetes diagnosis and those not having a diabetes diagnosis. Remaining analysis was limited to cases having a diabetes diagnosis. In order to determine population-based rates of ER visits, annual population estimates were obtained for 2005–2009 [30] and 2010-2014 [31]. Rates of visits per 100,000 population were calculated for visits with any diabetes diagnosis as well as rates for visits in which diabetes was the primary diagnosis.
Differences in patient, hospital, and area-based summary characteristics were first examined comparing those which had diabetes as a primary diagnosis compared to diabetes as a secondary diagnosis. Differences were assessed using the chi-square test for categorical variables and t-test for continuous variables. Next, multivariable logistic regression was used to examine the joint effect of all variables on discharge status, non-routine vs. routine. Data processing and analysis were performed using SAS 9.4 software (SAS Institute, Gary, North Carolina). This research was considered exempt from Institutional Review Board review at Loma Linda University due to being analysis of public-use data.
Results
Between 2005 and 2014 the estimated California population increased modestly from 36 million to 38.7 million. During this time the number of ER visits with a diabetes diagnosis nearly tripled from 342,106 in 2005 to 1,008,154 in 2014. Figure 1 converts these numbers to population-based rates to visualize the dramatic increase patients having a diabetes diagnosis. The overall rate jumped from 951 visits per 100,000 population in 2005 to 2,603 visits per 100,000 in 2014. However, the increase in ER visits which had a primary diagnosis of diabetes was much less dramatic, rising from a rate of 155 per 100,000 population in 2005 to 209 per 100,000 in 2014.
Figure 2 shows that between 2005 and 2014, ER visits for those with a mental health diagnosis increased steadily from 7.7% to 13.3% among visits which did not have a diabetes diagnosis. However, among ER visits for those who had a diabetes diagnosis, the percentage of co-occurring mental illness increased from 10.1% to 19.5%.
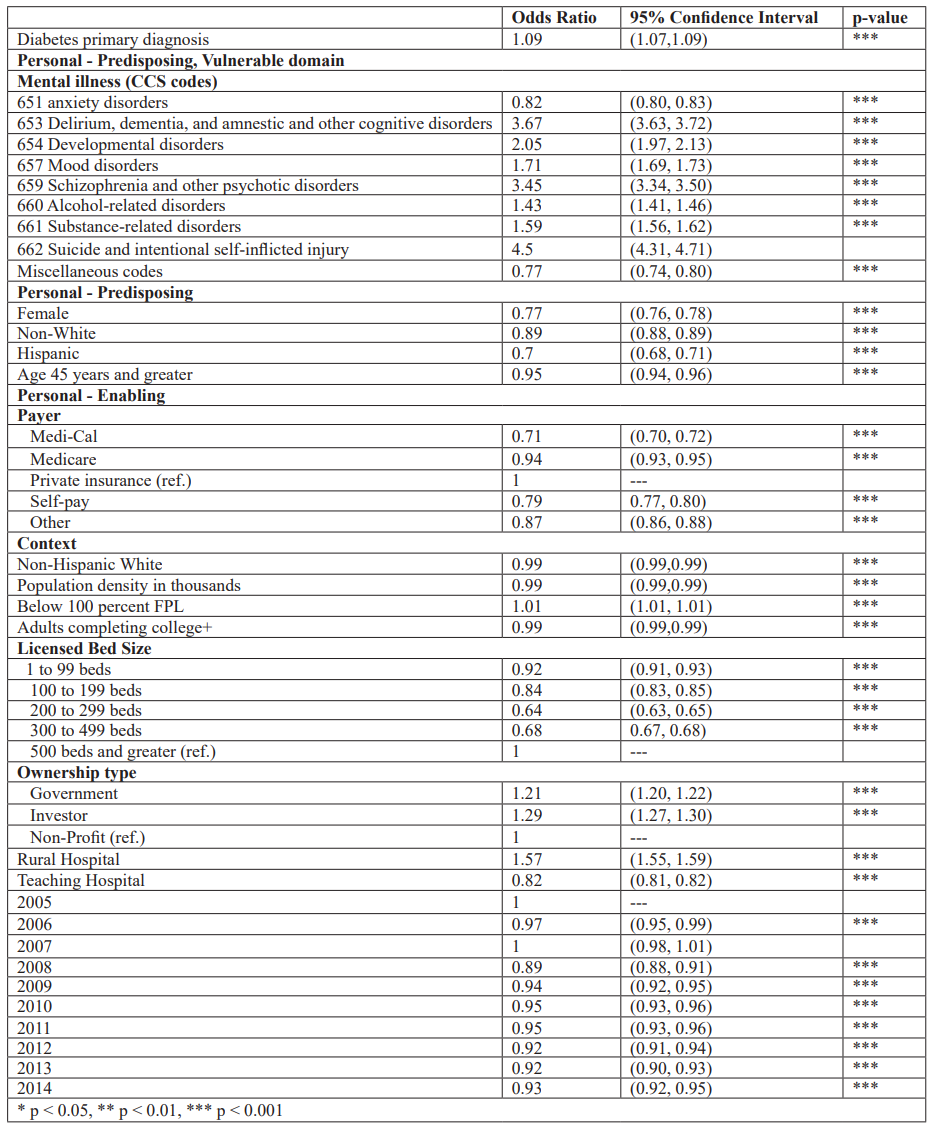
Table 1 presents characteristics of the 6.48 million ER visits in California between 2005 and 2014 which had a diabetes diagnosis. Of these, 10.76% had diabetes as a primary diagnosis and 15.81% had any mental diagnosis – the most common being mood or anxiety disorders. The majority of visits were for whites and those 45 years of age, with slightly more than half being for females. Particularly given the large sample size, there were significant (p<0.001) differences for all characteristics between those having diabetes as a primary vs. secondary diagnosis. Those with diabetes as a secondary diagnosis were more likely to have a mental diagnosis, to live in an area with a higher population percentage of non-Hispanic whites, and to be covered by private insurance or Medicare. Those with diabetes as a primary diagnosis were more likely to be self-pay and be seen at government / teaching hospitals. A non-routine discharge status was observed for 8.5% of those who had diabetes as a primary diagnosis compared to 8.14% of those with secondary diabetes diagnosis.
Table 2 presents predictors of non-routine discharges, i.e., everything other than being sent home. All predictors were significant at p<0.001, except for one of the calendar years. Several of the mental categories had the highest odds ratios, particularly suicide/self-harm (OR 4.5), delirium/dementia (OR 3.67) and schizophrenia (OR 3.45). Other notable variables associated with increased likelihood include being seen at a rural hospital (OR 1.57), an investor-owned or government hospital (OR 1.29 and 1.21, respectively), or having diabetes as the primary diagnoses (OR 1.09). On the other hand, factors associated with reduced likelihood of a non-routine discharge were being female, non-white, Hispanic, or 45 years of age; having any payer type other than private insurance; or being seen at a teaching hospital or any hospital having fewer than 500 beds.
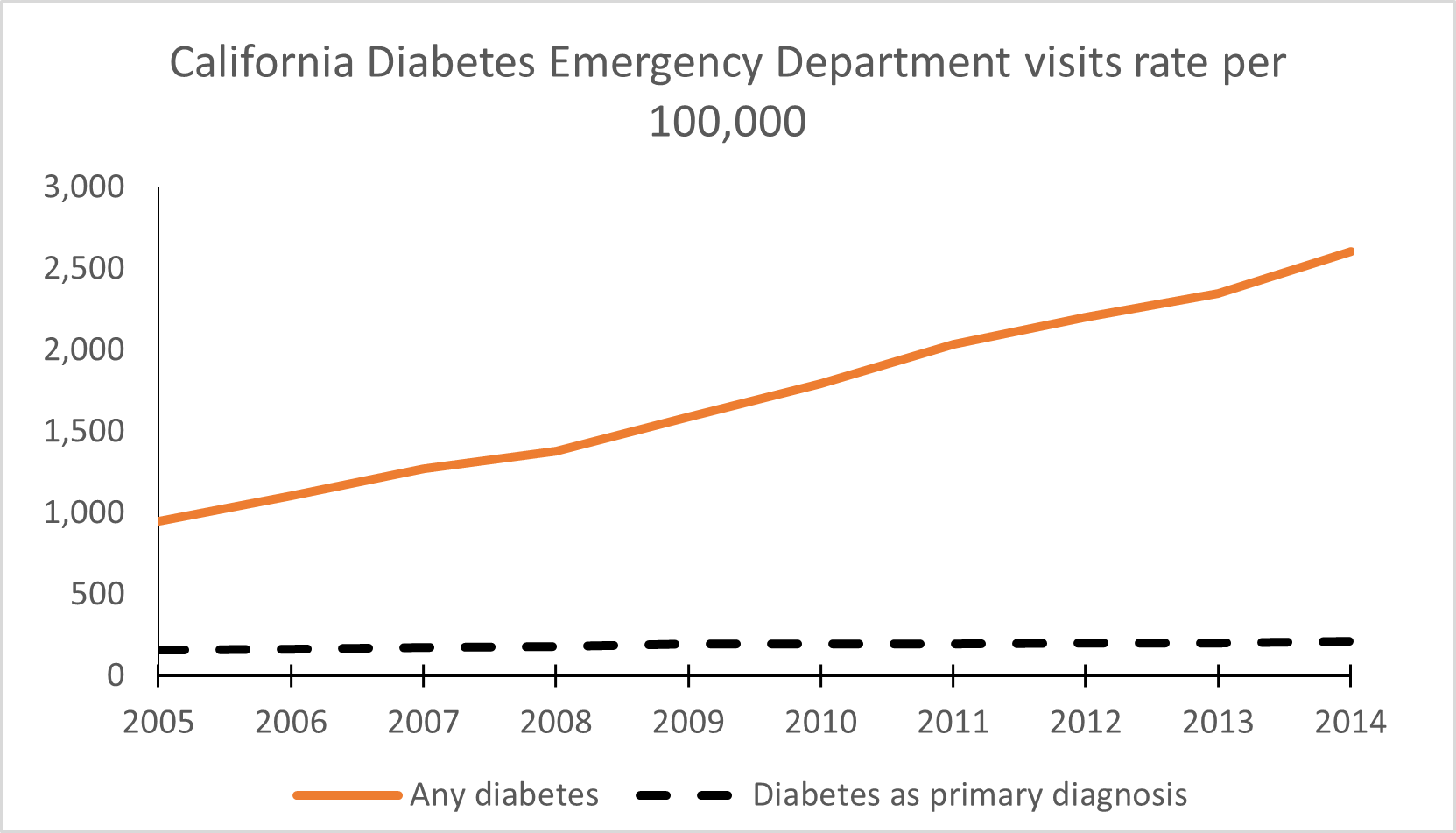
Figure 1: California diabetes emergency department visits, rate per 100,000.
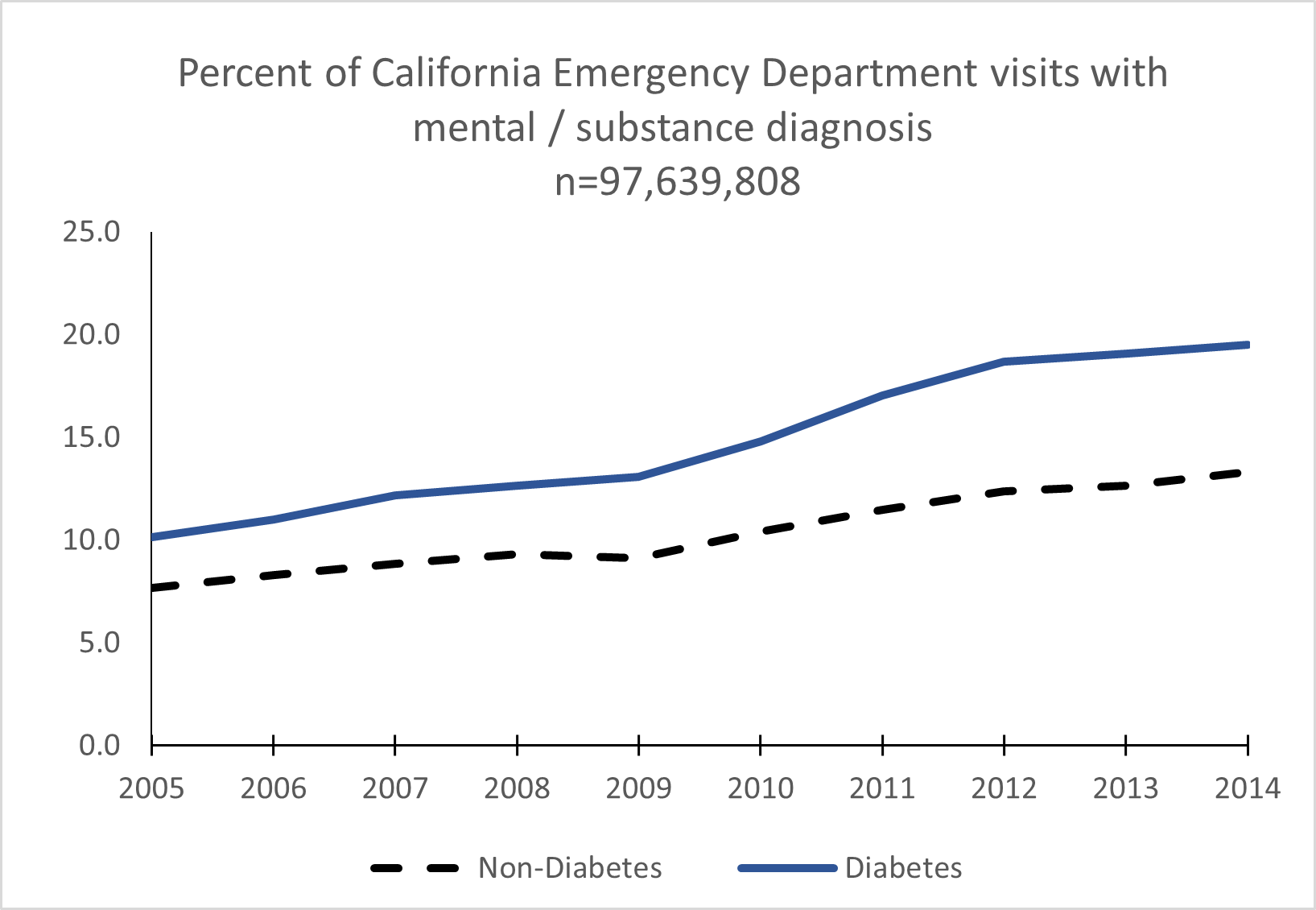
Figure 2: Percentage of California emergency department visits having a mental illness/substance use diagnosis (n=97,639,808).
Table 1: Descriptives for California Emergency Department visits, 2005-2014.

Table 2: Predictors of hospitalization among diabetes-related California Emergency Department visits, 2005-2014.
Discussion
Between 2005 and 2014 there were nearly 100 million ER visits in California, of which 6.5 million had a diabetes diagnosis. The annual rate of ER visits per 100,000 people for cases with a diabetes diagnosis jumped by 174% between 2005 and 2014. During this time the percentage of cases with co-occurring mental illness increased more rapidly among diabetes cases (10.1% to 19.5%) than among all other ER visits (7.7% to 13.3%).
This rapid rise in the number of ER visits in the U.S. with a secondary diagnosis of diabetes is due in part to increasing prevalence in the population, with the proportion of people diagnosed with diabetes increased from 5.61% in 2005 to 13.1% in 2016 [1]. Though the California increase in mental health and substance use disorder diagnoses in Emergency Departments is larger, it is consistent with studies based on the National Hospital Ambulatory Medical Care Survey. One study found an 8% increase between 2012-2015 [32] and another found a 30.6% increase between 2006 to 2015 [33].
The increase in the number of patients using Emergency Department services may be partially attributed to the fact that more people have received healthcare coverage under the Affordable Care Act (ACA), which was passed in 2010 and implemented in 2014 [34]. Part of the increase in the number of patients with a mental or substance disorder using ED services may be due to the Mental Health Parity and Addiction Equity Act of 2008, though most have found modest overall impacts in utilization [35].
Mood disorders, primarily depression, was the single most common type of psychiatric diagnosis identified among diabetes-related visits. Patients with that comobordity were more likely to be hospitalized or transferred. However, patients with self-harm/suicide attempt or psychotic disorders were even more likely to be hospitalized or transferred. This indicated need for better screening and treatment for behavioral health among diabetes patients. These results are consistent with findings that adults with diabetes have a 20% increase in prevalence of anxiety disorders compared to those without diabetes [14]. Anxiety can worsen diabetes self-care and also be exacerbated by fears regarding long-term complications [3]. Furthermore, others have found that women with diabetes are at greater risk for having anxiety [14]. However, depression exacerbates the comorbidities, and can lead to increased lack of adherence to medical modalities, and patients with depression and diabetes are more likely to utilize emergency department services [36]. Furthermore, individuals with a mental diagnosis are more likely to repeat users of emergency department services [37]. Looking beyond data of this study, though nationally there was a drop in ED visits during 2020 due to COVID-19 [38], the number of mental health-related ED visits increased in 2020 compared to the previous year [39].
Roughly 20% of diabetes-related visits were funded primarily by Medicaid / Medi-Cal. However, those with Medi-Cal funding were the least likely to be admitted to the hospital. This higher frequency of visits compared to admissions may indicate a lower quality of diabetes care among Medi-Cal funded patients with mental illness [40,41]. In fact, a recent analysis of Kaiser Permanente Northern California data revealed that patients with diabetes and comorbid serious mental illness actually had better diabetes control compared to those not having SMI [42].
Historically, it was estimated that as many as 45% of diabetic patients had undetected mental health disorders [43], with treatment exacerbated by fragmentation between primary and behavioral health care. Efforts to minimize the rising use of Emergency Department Services by those having both diabetes and mental illness or substance use disorders include integration of primary care and behavioral services so that physicians work collaboratively with other mental health professionals to treat patients with comorbid diseases. A major approach is rereferred to as Collaborative Care [44] or the Interdisciplinary Team Approach to Healthcare [45]. The collaborative / integrative model of primary care and behavioral health can lead to better outcomes and quality of life, and there are models for financial sustainability [46]. As one example, in order to better deal with patients having complex issues, such as a major medical illness, mental illness, and homelessness, the Zuckerberg San Francisco General Hospital Emergency Department created a Social Medicine team. Using hospital resources and funding County and federal grant funds, they were able to better deal with needs of patients and reduce hospitalizations [47].
It is recommended that physicians routinely screen for common psychiatric disorders using brief, validated instruments such as the patient health questionnaire (PHQ) and symptom checklist-90 (SCL-90) [48]. Even in an emergency setting one can use simple screening tools such as the Beck Depression Inventory or the Center for Epidemiologic Studies Depression Scale [49]. Upon identification, evidence-based psychological interventions such as cognitive-behavior therapy, problem-solving therapy, counseling, or brief psychodynamic psychotherapy can reduce stress and improve coping in those with chronic illnesses and are correlated with reduced glycosylated hemoglobin A1c (HbA1c) levels in both types of diabetes [50]. There have been new interventions such as group-based therapy, online treatment, and exercise, which have been found to be effective for depression, but not always for glycemic control [51-59].
Limitations
Although this research has reached its aims, there were some limitations. Though the data presented used socio-demographic information, this research did not evaluate statistics of race, ethnicity, gender, or income as they may pertain to both mental health disparities and diabetes in the results. Masked data for years 2005-2011 and missing data for demographics in years 2012-2014 and resulting for imputation and may have biased findings, particularly under-representing potential impacts. The data present also does not consider social factors that may affect the increase of hospital utilization such as improved access to care. Though the majority of cases were Type II diabetes, we did not formally break out Type I vs. Type II. The de-identified nature of data did not allow accounting for individuals having multiple visits.
Conclusion
Diabetes became much more commonly diagnosed within California Emergency Rooms between 2005 and 2014. The percent of mental illness and substance use disorder diagnosed among diabetes-related visits increased more rapidly compared to non-diabetes visits. Those individuals having a handful of different mental illness were more likely to admitted or transferred compared to individuals diagnosed with diabetes who did not have a diagnosed mental illness. Higher rates of treated and released discharge status among those with public insurance or self-pay suggests suboptimal outpatient care compared to those having private insurance. This suggests need for improved primary care as well as better coordination with behavioral health.
Financial Support: The authors received no financial support regarding this article.
Financial/nonfinancial disclosures: For all authors, no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Other contributions: The work was performed at Loma Linda University.
References
- Centers for Disease Control and Prevention. National Diabetes statistics report. Centers for Disease Control and Prevention, 2020.
- Lin J, Thompson TJ, Cheng YJ, et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metrics, 2018; 16: 9. https://doi.org/10.1186/s12963-018-0166-4
- Bickett A, Tapp H. Anxiety and diabetes: Innovative approaches to management in primary care. Experimental biology and medicine (Maywood, N.J.), 2016; 241(15): 1724–1731. https://doi.org/10.1177/1535370216657613
- American Diabetes Association. The cost of Diabetes. Economic costs of Diabetes in the U.S. in 2017, 2018.
- Roehrig C. Mental Disorders Top the List Of The Most Costly Conditions In The United States: $201 Billion. Health Affairs; 2016; 35(6): 1130–1135. doi: 10.1377/hlthaff.2015.1659
- National Alliance for the Mentally Ill. Webpage Mental Health by the numbers, 2020.
- Rockville HCUP Fast Stats. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality, 2021.
- Hall MJ, Rui P, Schwartzman A. Emergency department visits by patients aged 45 and over with diabetes: United States, 2015. NCHS Data Brief, no 301. Hyattsville, MD: National Center for Health Statistics, 2018.
- Santillanes G, Axeen S, Chun Nok Lam CN, Michael Menchine M. National trends in mental health-related emergency department visits by children and adults, 2009–2015. The American Journal of Emergency Medicine, 2020; 38(12): 2536-2544, https://doi.org/10.1016/j.ajem.2019.12.035.
- Parihar HS, Thakar H, Hongjun Y, Allen S. Is depression an independent risk factor for the onset of Type 2 diabetes mellitus? Drug Development & Therapeutics, 2016; 7(2): 75-80. doi:10.4103/2394-6555.191148
- Sacco W, Bykowski C, Mayhew L. Pain and functional impairment as mediators of the link between medical symptoms and depression in type 2 diabetes. International Journal of Behavioral Medicine, 2013; 20(1): 22-29. doi:10.1007/s12529-011-9210-5
- Mental Health America. Co-occurring disorders and depression, 2016.
- Stubbs B, Vancampfort D, De Hert M, Mitchell AJ. The prevalence and predictors of type two diabetes mellitus in people with schizophrenia: a systematic review and comparative meta-analysis. Acta Psychiatrica Scandinavica, 2015; 132(2): 144-157. doi:10.1111/acps.12439
- de Groot M, Golden SH, Wagner J. Psychological conditions in adults with diabetes. American Psychologist, 2016; 71(7): 552-562. doi:10.1037/a0040408
- Robinson M-E, Simard M, Larocque I, Shah J, Nakhla M, Rahme E. Risk of Psychiatric Disorders and Suicide Attempts in Emerging Adults with Diabetes. Diabetes Care, 2020; 43(2): 484–486. https://0-doi-org.catalog.llu.edu/10.2337/dc19-1487
- Wu CS, Lai MS, Gau SS. Complications and mortality in patients with schizophrenia and diabetes: population-based cohort study. Br J Psychiatry, 2015; 207: 450–457.
- Holt RI, Mitchell AJ. Diabetes mellitus and severe mental illness: Mechanisms and clinical implications. Nature Reviews Endocrinology, 2015; 11(2): 79-89. doi:10.1038/nrendo.2015.203
- Desai R, Nayak R. Effects of Medication Nonadherence and Comorbidity on Health Resource Utilization in Schizophrenia. Journal of managed care & specialty pharmacy, 2019; 25(1): 37–46. https://doi.org/10.18553/jmcp.2019.25.1.037
- Ajuwon AM, Love R. Type 2 diabetes and depression in the African American population. Journal of the American Association of Nurse Practitioners, 2020; 32(2): 120–127. https://0-doi-org.catalog.llu.edu/10.1097/JXX.0000000000000240
- OSHPDa: Office of Statewide Health Planning and Development. Healthcare information division: Emergency department data sets and data products, 2016.
- United States Census Bureau, My Congressional District, 2016.
- Medical Service Study Areas (MSSA), 2016.
- OSHPD: Office of Statewide Health Planning and Development.Healthcare Utilization, 2016.
- Appendix A - Clinical classification software-DIAGNOSES, 2013.
- Andersen RM, Davidson PL and Baumeister SE. Improving access to care In: Kominsky GF (ed) Changing the U.S. Health Care System: Key Issues in Health Services Policy and Management. Third ed. San Francisco: Jossey-Bass, 2014; 33-69.
- Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Services Research, 2000; 34(6): 1273–1302.
- Allison PD. Missing Data. Thousand Oaks, CA: Sage, 2002.
- Banta JE, Joshi KP, Beeson L, Nguyen HB. Patient and hospital characteristics associated with inpatient severe sepsis mortality in California, 2005-2010. Critical Care Medicine, 2012; 40(11): 2960-2966.
- Banta JE, McKinney O. Faith-based hospitals and variation in psychiatric inpatient length of stay in California, 2002-2011. Journal of Religion and Health, 2016; 55(3): 787-802.
- State of California, Department of Finance, California county population estimates and components of change by year, July 1, 2000-2010. Sacramento, California, 2011.
- State of California, Department of Finance, E-2. California county population estimates and components of change by year — July 1, 2010–2015, 2015.
- Downey LVA, Hong A, Herrera K. Changes in Proportions of Emergency Department Patients with Mental Illness Noted in the National Hospital Ambulatory Medical Care Survey, 2012-2015. Southern Medical Journal, 2020; 113(2): 51–54.
- Nam E, Lee E, Kim H. 10-Year Trends of Emergency Department Visits, Wait Time, and Length of Stay among Adults with Mental Health and Substance use Disorders in the United States. The Psychiatric quarterly, 2021. DOI: 10.1007/s11126-021-09894-y.
- Yanuck J. The Affordable Care Act: Disparities in emergency department use for mental health diagnoses in young adults. World Journal of Emergency Medicine, 2017; 8(3): 206. doi:10.5847/wjem.j.1920-8642.2017.03.008
- Drake C, Busch SH, Golberstein E. The Effects of Federal Parity on Mental Health Services Use and Spending: Evidence from the Medical Expenditure Panel Survey. Psychiatric services (Washington, D.C.), 2019; 70(4): 287–293. https://doi.org/10.1176/appi.ps.201800313
- Ingram WM, Weston C, Ritchie MD, Larson S. Depression linked to frequent emergency department use in large 10-year retrospective analysis of an integrated health care system, 2017. doi:10.1101/115238
- Niedzwiecki MJ, Sharma PJ, Kanzaria HK, McConville S, Hsia RY. Factors Associated with Emergency Department Use by Patients with and Without Mental Health Diagnoses. JAMA Netw Open, 2018; 1(6): e183528. doi:10.1001/jamanetworkopen.2018.3528
- Kim HS, Cruz DS, Conrardy MJ, Gandhi KR, Seltzer JA, Loftus TM, et al. Emergency Department Visits for Serious Diagnoses During the COVID‐19 Pandemic. Academic Emergency Medicine, 2020; 27(9): 910–913. https://0-doi-org.catalog.llu.edu/10.1111/acem.14099
- Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US Emergency Department Visits for Mental Health, Overdose, and Violence Outcomes Before and During the COVID-19 Pandemic. JAMA Psychiatry, 2021; 78(4): 372–379. doi:10.1001/jamapsychiatry.2020.4402
- Williams SL, Haskard KB, Banta JE, Haviland MG, DiMatteo MR, Werner LS, et al. Serious mental illness and diabetes care among California adults. The International Journal of Psychiatry in Medicine, 2010; 40(3): 233-245.
- Banta JE, Morrato EH, Lee SW, Haviland MG. Retrospective Analysis of Diabetes Care in California Medicaid Patients with Mental Illness. Journal of General Internal Medicine, 2009; 24(7): 802-808.
- Mangurian C, Schillinger D, Newcomer JW, Vittinghoff E, Essock S, Zhu Z, et al. Comorbid Diabetes and Severe Mental Illness: Outcomes in an Integrated Health Care Delivery System. JGIM: Journal of General Internal Medicine, 2020; 35(1): 160–166. https://0-doi-org.catalog.llu.edu/10.1007/s11606-019-05489-3
- Frayne S, Halanych J, Miller D. Disparities in diabetes care impact of mental illness. JAMA Internal Medicine, 2005; 165(22): 2631-2638. doi: 10.1001/archinte.165.22.2631
- Unützer J, Harbin H, Schoenbaum M, Druss B. The collaborative care model: An approach for integrating physical and mental health care in Medicaid health homes. Centers for Medicare & Medicaid Services, 2013.
- Mayo AT, Woolley AW. Teamwork in health care: maximizing collective intelligence via inclusive collaboration and open communication. Journal of Ethics: American Medical Association, 2016.
- Heilbrun A, Drossos T. Evidence for Mental Health Contributions to Medical Care in Diabetes Management: Economic and Professional Considerations. Curr Diab Rep, 2020; 20: 79. https://0-doi-org.catalog.llu.edu/10.1007/s11892-020-01337-5
- Chase J, Bilinski J, Kanzaria HK. Caring for Emergency Department Patients with Complex Medical, Behavioral Health, and Social Needs. JAMA: Journal of the American Medical Association, 2020; 324(24): 2550–2551. https://0-doi-org.catalog.llu.edu/10.1001/jama.2020.17017
- Balhara YP. Diabetes and psychiatric disorders. Indian Journal of Endocrinology and Metabolism, 2011; 15(4): 274-283. doi:10.4103/2230-8210.85579
- Ducat L, Philipson LH, Anderson B. The mental health comorbidities of diabetes. National Center for Biotechnology Information, 2014. doi:10.1001/jama.2014.8040
- Markowitz SM, Gonzalez JS, Wilkinson JL, Safren SA. A review of treating depression in diabetes: Emerging findings. Psychosomatics, 2011; 52(1): 1-18. doi: 10.1016/j.psym.2010.11.007
- van der Feltz CC, Allen SF, Holt RIG, Roberts R, Nouwen A, Sartorius N. Treatment for comorbid depressive disorder or subthreshold depression in diabetes mellitus: Systematic review and meta‐analysis. Brain & Behavior, 2021; 11(2): 1–25. https://0-doi-org.catalog.llu.edu/10.1002/brb3.1981
- Beckles GL, Chiu-Fang C. Diabetes -- United States, 2006 and 2010. MMWR: Morbidity & Mortality Weekly Report, 2013; 62: 99-104.
- Beckles GL, Chiu-Fang C, Chou C-F. Disparities in the prevalence of diagnosed diabetes - United States, 1999-2002 and 2011-2014. MMWR: Morbidity & Mortality Weekly Report, 2016; 65(45): 1265-1269. doi:10.15585/mmwr.mm6545a4
- Haynes-Maslow L, Leone LA. Examining the relationship between the food environment and adult diabetes prevalence by county economic and racial composition: an ecological study. BMC public health, 2017; 17(1): 648.
- Iheanacho T, Rosenheck R. Prevalence and correlates of diabetes mellitus among homeless veterans nationally in the Veterans Health Administration. Journal of Social Distress & the Homeless, 2016; 25(2): 53-59. doi:10.1080/10530789.2016.1169722
- Mier N, Wang X, Smith ML, Irizarry D, Treviño L, Alen M, et al. Factors influencing health care utilization in older Hispanics with diabetes along the Texas-Mexico border. Population Health Management, 2012; 15(3): 149-156. doi:10.1089/pop.2011.0044
- OSHPDb: Office of Statewide Health Planning and Development. Healthcare information division: Hospital annual utilization data, 2016.
- Saydah SH, Imperatore G, Beckles GL. Socioeconomic status and mortality: Contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care, 2013; 36(1): 49-55. doi:10.2337/dc11-1864
- Yuan Y. Multiple imputation for missing data: Concepts and new development. Rockville, MD: SAS Institute Inc., 2005.

