A Proposal of COVID-19 Eradication Measures in the Herd Immunity Setting, Favourable to SARS-CoV-2 Variants of Reduced Detection by the Prevailing Immune Response
Sven Kurbel*
Josip Juraj Strossmayer University of Osijek, Medical Faculty, J Huttlera 4, Osijek 31000, Croatia
Polyclinic Aviva Zagreb, Nemetova 2, Zagreb 10000, Croatia
Received Date: 30/08/2023; Published Date: 22/01/2024
*Corresponding author: Sven Kurbel, Josip Juraj Strossmayer University of Osijek, Medical Faculty, J Huttlera 4, Osijek 31000, Croatia; Polyclinic Aviva Zagreb, Nemetova 2, Zagreb 10000, Croatia
Abstract
COVID-19 eradication has been proposed and considered being more feasible than the polio eradication, but less than the smallpox eradication. The actual measures, their timing and applicability remain to be defined.
Emergence of new SARS-CoV-2 variants in the initial host requires sufficient viral multiplication and presence in respiratory fluids, as prerequisites of infecting other persons. As long as susceptible people are exposed, new viral variants are selected for higher infectivity, until the setting of herd immunity is nearby.
In a population approaching the herd immunity, few new cases form clusters, allowing several viral variants to coexist and evolve separately, until a new variant with a reduced recognition by the prevailing immune response starts a new pandemic that spread among all people regardless of their convalescence or previous vaccines.
The proposed COVID-19 eradication can start by regular tests of humoral and cellular immunity against COVID-19. Susceptible persons should have two options: vaccination, or to remain isolated from other susceptible people. These measures would make a setting of enhanced herd immunity. Several years of regular implementation of these measures might gradually reduce the number of new COVID-19 cases, until the COVID-19 risk is gone.
Keywords: COVID-19; SARS-CoV-2; Eradication measures; Herd immunity; Humoral immunity cellular immunity
Introduction
The burden of COVID-19 on economy and society is so enormous that any proposal for COVID-19 eradication is understandable and worth of support. The global COVID-19 eradication was recently evaluated [1] and considered being slightly more feasible than the future polio eradication, but much less than the already accomplished smallpox eradication. Several challenges are listed: high vaccination coverage; possible need to update vaccine designs; complex implementation of public health and social measures [1]. It has been concluded that a more formal expert review of this topic is required by international bodies.
An earlier proposal of COVID-19 eradication [2] was based on similarities between smallpox and COVID-19 characteristics (high reproduction number, combination of case clustering and superspreading during social gatherings). The authors have suggested that measures applied during the smallpox eradication can be used for COVID-19, although COVID-19 often result in mild disease that still enables viral transmission. Several measures are proposed: containment by stringent public health measures; enhanced testing to identify cases with their contacts; vaccination against SARS-CoV-2 [2].
Actions against smallpox have started in 1958, relaunched by the WHO in 1967 and finished in 1977. Since the days of smallpox, available health care resources are substantially improved, suggesting that the eradication of SARS-CoV might be done comparatively faster, although the timing and types of measures needed for this tremendous task remain to be defined.
Model of emergence of new SARS-CoV-2 variants
COVID-19 pandemic shows a rapid succession of dominant viral SARS-CoV-2 variants [3], probably caused by intrinsically high mutation rates in RNA viruses [4]. New variants are seemingly always more infective than the previous, enabling the pandemic to move around the globe in waves directed by the local availability of susceptible individuals among contacts of COVID-19 patients.
For microbes and viruses, the decisive survival challenges are within their hosts. Individual immune response and other intrinsic settings force pathogens to change or to be eliminated, often replaced by a more resilient pathogen. Probable survival and spreading challenges for new SARS-CoV-2 variants in different population settings are listed in Table 1. The initial idea is that mutated viral variants can emerge only during the infection of a host that was susceptible to previously present SARS-CoV-2 variants. In other words, any mutation that promotes a new SARS-CoV-2 variant occurs in COVID-19 patients during the infection.
Survival challenges for the new, mutated viral variant within the initial host can be divided in phases (Table 1): the replication challenge requires sufficient viral multiplication in normal ACE2 expressing cells, while the excretion challenge requires sufficient viral presence in respiratory and digestive fluids [5]. Both challenges depend on two relations: competition with the coexisting unmutated viral variant and on the emerging immune response of the initial host against both variants.
Competition between the mutated and the unmutated variant for replication and excretion forces the new SARS-CoV-2 variant to remain ACE2 dependent. Otherwise, it would lose the ability to compete with the unmutated variant for cellular replication in ACE2 expressing cells of the initial host. Replications of all new viral variants thus seem inevitably linked to the dysfunction of the renin-angiotensin system, more often and severe in older patients with stress-related comorbidities [6].
The third survival challenge for the new viral variant is to infect other persons, beside the initial host. This challenge is easily reduced by various epidemiological and social measures, presence of already immune persons (convalescent or vaccinated) among available contacts, and other viral variants.
In the early phase of local epidemic, the challenge of infectivity favours increased spreading among susceptible persons (unvaccinated or not convalescent persons, or those with already diminished previous immune response to this virus). Specific immune response against the previous SARS-CoV-2 variant can also prevent clinical disease by some new variants [7], although often not completely.
If one of the emerging new variants can evade the prevailing immune response [8, 9], it can probably easily spread to other persons, despite their vaccination or convalescence. The emergence of a “stealth” SARS-CoV-2 variant is a critical scenario that leads to self-sustained COVID-19 pandemic.
It is here proposed that in areas approaching the herd immunity, the speed of viral spreading might become unimportant, due to very few susceptible persons. In this setting, new cases are often clustered and this allows several viral variants to coexist in the same population and evolve separately. The infection starts to imitate an endemic disease with stable total numbers of new cases, since this setting forces the emerging viral variant to evolve toward reduced recognition by the prevailing immune response in the population (Figure 1).
This hypothetical endemic setting can last until an immunologically different viral variant emerges, less detectable by available immune responses. When this “stealth” variant occurs, it can spread like a new disease that requires new vaccines and social measures.
This interpretation suggests that the COVID-19 pandemic have a potential to initiate slow cycles of ever returning new SARS-CoV-2 variants (Figure 1), thus leading to a perpetuating Corona pandemic.
Table 1: Three proposed survival challenges for the new viral variant within the initial host that acquired infection with the previous SARS-CoV-2 variant: a/ the replication challenge is sufficient viral multiplication in ACE2 expressing cells; b/ the excretion challenge is sufficient viral presence in respiratory and digestive fluids; c/ infecting other persons in contact with the initial host.

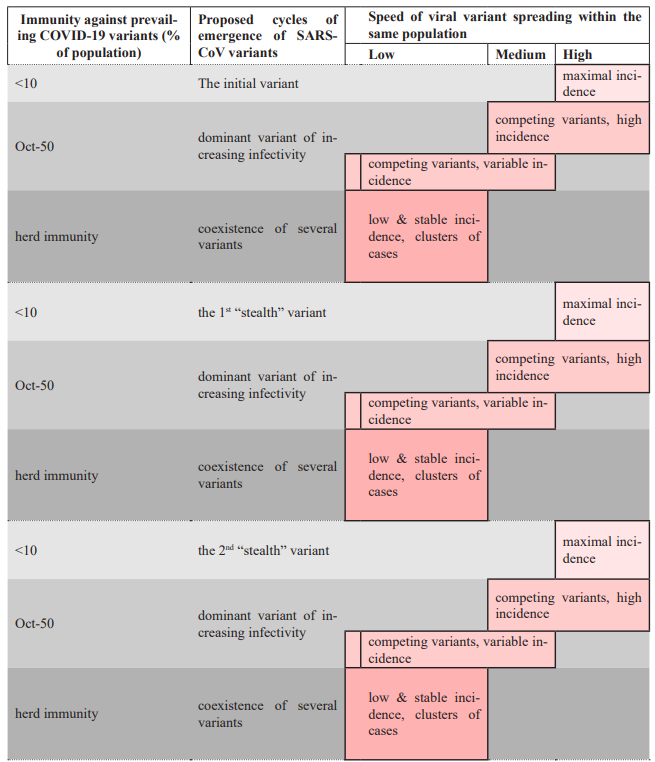
Figure 1: A proposed model for the transition of the COVID-19 pandemic to a cyclical pandemic, due to emergence of viral variants of altered antigenicity. These “stealth” variants can act as new pathogens and restart the pandemic story (measures, new vaccines etc.). Due to survival pressure described in the main text, these dangerous variants are expected to emerge in populations approaching herd immunity. This risk strongly supports global efforts for SARS-CoV-2 eradication.
Proposed modalities of SARS-CoV-2 eradication: focus on individual immunity
Based on Table 1, it seems that areas with already high vaccination and convalescence rates are particularly prone to develop a new “stealth” variant due to coexistence of several coexisting clones that independently replicate in small case clusters. COVID-19 eradication can start in these areas by regular tests of population immunity against COVID-19 (one or two times per year):
! The first line tests for all persons: SARS-CoV-2 IgG antibodies;
" The second line tests for all persons with absent or low SARS-CoV-2 IgG antibodies: tests of cellular immunity against SARS-CoV-2 (e.g., similar to methods in ref. [10]).
All detected COVID-19 susceptible persons (lacking sufficient humoral and cellular response to SARS-CoV-2) should have a choice of two options:
" another vaccination against SARS-CoV-2
OR
" sustained restricted social contact with other COVID-19 susceptible persons.
This simple transfer of our focus from the virus occurrence to the recognition of remaining susceptible persons, can make new cases much less likely. If susceptible individuals get vaccinated or remain isolated from other susceptible people, these measures would make a setting of enhanced herd immunity. Several years of regular implementation of these measures might gradually reduce the number of new COVID-19 cases, until the COVID-19 risk is gone.
Conclusive remarks
Risk of facing another cycle of Corona pandemic that demands development and global availability of new vaccines should be a strong argument to implement eradication measures for SARS-CoV-2 in all countries approaching herd immunity. Detection of remaining susceptible individuals should be started in populations with high proportions of people immune to COVID-19, by vaccination or convalescence.
If the public is regularly informed about the current number of hospitalised COVID-19 patients and on numbers of immune and susceptible persons, even a lay person would understand how far we should go in our epidemiological and social measures.
Regular testing of immunity against COVID-19 in all inhabitants would allow selective public actions against virus spreading and protection of the susceptible minority. It seems as a good alternative to the current EU policy of issuing “COVID-19 Passports” of arbitrarily declared validity duration.
Any COVID-19 susceptible person can decide whether to take another vaccine dose, or to remain isolated from other COVID-19 susceptible persons.
It has been recently suggested that thousands of SARS-CoV-2 variants of concern might have passed unnoticed, because they have died out before having the opportunity to emerge in the population [11]. Currently important Delta COVID-19 variant was identified in India in October 2020, while "Delta Plus" variant was found in June 2021 [12]. Both are more infectious than previous variants, suggesting that they originated in populations with many COVID-19 susceptible individuals. Their fast spreading probably suppresses any "stealth" variants that might have already occurred somewhere in the world, as suggested [11].
Acknowledgments:
This Commentary is among activities financed through grant VIF2018MEFOS02 from the Croatian Ministry of Science, Education and Sport.
The Author declares no conflict of interest regarding the content of this manuscript.
References
- Wilson N, Mansoor OD, Boyd MJ, Kvalsvig A, Baker MG. We should not dismiss the possibility of eradicating COVID-19: comparisons with smallpox and polio. BMJ Glob Health, 2021; 6(8): e006810. doi: 10.1136/bmjgh-2021-006810.
- Heymann DL, Wilder-Smith A. Successful smallpox eradication: what can we learn to control COVID-19? J Travel Med, 2020; 27(4): taaa090. doi: 10.1093/jtm/taaa090.
- Singh J, Pandit P, McArthur AG, Banerjee A, Mossman K. Evolutionary trajectory of SARS-CoV-2 and emerging variants. Virol J, 2021; 18(1):166. doi: 10.1186/s12985-021-01633-w.
- Duffy S. Why are RNA virus mutation rates so damn high? PLoS Biol, 2018; 16(8): e3000003. doi: 10.1371/journal.pbio.3000003.
- Mehraeen E, Salehi MA, Behnezhad F, Moghaddam HR, SeyedAlinaghi S. Transmission Modes of COVID-19: A Systematic Review. Infect Disord Drug Targets, 2020. doi: 10.2174/1871526520666201116095934.
- Kurbel S. The renin-angiotensin system in COVID-19: Why ACE2 targeting by coronaviruses produces higher mortality in elderly hypertensive patients? Bioessays, 2021; 43(3): e2000112. doi: 10.1002/bies.202000112.
- Martínez-Flores D, Zepeda-Cervantes J, Cruz-Reséndiz A, Aguirre-Sampieri S, Sampieri A, Vaca L. SARS-CoV-2 Vaccines Based on the Spike Glycoprotein and Implications of New Viral Variants. Front Immunol. 2021; 12: 701501. doi: 10.3389/fimmu.2021.701501.
- Rehman SU, Rehman SU, Yoo HH. COVID-19 challenges and its therapeutics. Biomed Pharmacother, 2021; 142: 112015. doi: 10.1016/j.biopha.2021.112015.
- Raman R, Patel KJ, Ranjan K. COVID-19: Unmasking Emerging SARS-CoV-2 Variants, Vaccines and Therapeutic Strategies. Biomolecules, 2021; 11(7): 993. doi: 10.3390/biom11070993.
- Lineburg KE, Neller MA, Ambalathingal GR, Le Texier L, Raju J, Swaminathan S, et al. Rapid whole-blood assay to detect SARS-CoV-2-specific memory T-cell immunity following a single dose of AstraZeneca ChAdOx1-S COVID-19 vaccine. Clin Transl Immunology, 2021; 10(8): e1326. doi: 10.1002/cti2.1326.
- Gómez-Carballa A, Pardo-Seco J, Bello X, et al. Superspreading in the emergency of COVID-19 variants, Trends in Genetics 2021; https://doi.org/10.1016/j.tig.2021.09.003
- Kannan SR, Spratt AN, Cohen AR, Naqvi SH, Chand HS, Quinn TP, et al. Evolutionary analysis of the Delta and Delta Plus variants of the SARS-CoV-2 viruses. J Autoimmun, 2021; 124: 102715. doi: 10.1016/j.jaut.2021.102715.

