Association of Gastroesophageal Reflux Disease with Tachyarrhythmias and its Impact on Outcomes
Jose R Russe Russe1, Rezwan Munshi1, Chiya Abramowitz2,*, Ethan Shamsian2, James R Pellegrini Jr1, Kristen Farraj1, Aboud Kaliounji3 and Nisha Pillai4
1Department of Medicine, Nassau University Medical Center, NY, USA
2NYIT College of Osteopathic Medicine, Long Island, NY, USA
3St. George School of Medicine, West Indies, Grenada
4Department of Cardiology, Northwell Health, NY, USA
Received Date: 05/06/2023; Published Date: 23/10/2023
*Corresponding author: Chiya Abramowitz, MS3, NYIT College of Osteopathic Medicine, Long Island, 101 Northern Blvd, Glen Head, NY, USA
Abstract
Tachyarrhythmias (TA) and Gastroesophageal Reflux Disease (GERD) represent distinct pathologies affecting millions of Americans annually. However, recent studies have pointed to an association between GERD and a specific type of TA, atrial fibrillation (AFib). The reasons behind this association have yet to be defined. Still, various theories have been proposed, including an increased autonomic tone or regional inflammation resulting from GERD that may lead to a specific TA such as AFib. However, more information about the association between GERD and other TAs or the variables linked with such a relationship is needed. Our study seeks to develop the association between GERD and TA and compare the outcomes and associated factors between admitted GERD patients with and without TAs. The results showed that patients with GERD had higher odds of having TA than those without GERD. In addition, patients presenting with TA and GERD were older than patients without TA, though both cohorts are more likely to be female.
Furthermore, there was no significant difference in CCI between patients with GERD and TA compared to the non-TA cohort. Among patients presenting with GERD and TA, the most common cause of TA was atrial fibrillation (82.4%), followed by atrial flutter (10.2%) and SVT (7.3%). Patients with GERD and TA were found not to have higher mortality, length of hospital stay, or hospital charges. Further exploration is needed to identify GERD as an underlying etiology for such common arrhythmias and treat them appropriately to minimize TA-related complications.
Introduction
There is a common clinical link between tachyarrhythmias (TAs) and Gastroesophageal Reflux Disease (GERD). TAs are broadly classified as narrow-complex tachycardia (NCT; <120 ms) and wide-complex tachycardia (WCT; >120 ms). NCTs include paroxysmal sinus tachycardia, atrial flutter, atrial fibrillation (AFib), multifocal tachycardia, inappropriate sinus tachycardia, focal atrial tachycardia, Atrioventricular Nodal Reentrant Tachycardia (AVRT), sinoatrial nodal reentrant tachycardia, and orthodromic atrioventricular reciprocating tachycardia. WCTs include monomorphic ventricular tachycardia, aberrant Supraventricular Tachycardia (SVT), antidromic atrioventricular reciprocating tachycardia, polymorphic ventricular tachycardia, pre-excited AFib, artifactual tachycardia, AFib with aberrant conduction, and pacemaker-mediated tachycardia [1]. TAs can generally be divided into primary etiology due to cardiac injury or defective cardiac electrical conduction system or secondary etiology due to withdrawal syndromes, thyroid storm, pulmonary embolism, or sepsis. TAs typically present with palpitations, diaphoresis, dyspnea, chest pain, dizziness, syncope, and heart failure [1,2]. The most common TA is AFib affecting at least 2.3 million people in the United States (US) alone, followed by SVT, with nearly 90,000 cases detected annually, with ~25% requiring hospitalization [3].
GERD is a chronic gastrointestinal disorder characterized by the regurgitation of gastric contents into the esophagus that has a prevalence of up to 20% in the US [4]. Multiple and different mechanisms, including intrinsic, structural, or both, trigger GERD by disrupting the esophagogastric junction barrier manifesting. Symptoms of heartburn and regurgitation occur due to esophageal exposure to acidic gastric contents [4]. Typical symptoms of GERD include heartburn, regurgitation, globus sensation, dysphagia, and belching. In contrast, atypical symptoms are mainly extra-esophageal, including chest pain, dental erosions, chronic cough, laryngitis, or asthma [4,5].
Recently, research has elucidated the association between GERD and TA. Unfortunately, no conclusive understanding has been found regarding the reasoning behind the relationship; however, a few main mechanisms have been identified, specifically for the connection between GERD and AFib [6].
One such mechanism suggests GERD’s ability to create an imbalance in the autonomic tone. GERD’s increase in vagal tone has been more correlated to AFib than sympathetic tone, especially in spontaneous/paroxysmal Afib, which occurs more often in the healthier, younger population. The afferent vagal pathway is affected by increased stimulation of the esophageal mucosa. This stimulation reflexively decreases sinus node depolarization and atrioventricular conduction, creating the ideal situation for arrhythmias [6]. Another such mechanism proposes GERD’s inflammatory sequelae causing AFib. Acid reflux has been shown to release inflammatory mediators such as IL-1B, IL-6, and CRP, which lead to the incidence, defibrillation, recurrence, and prognosis of AFib via the complement pathway activation [6].
Additionally, regional inflammation induced by GERD in the proximal esophagus can affect the adjacent left atrium and cause local pericarditis or atrial myocarditis, leading to AFib [6]. A final mechanism suggests acid reflux induced by Hiatal hernias (HH) can bring about AFib. HH causes acid in the esophagus, further maintained by a more relaxed LES. A possible explanation for HH causing AFib is the pressure the hernia induces on the left atrium, which generates an ischemic left side of the heart. The decreased blood flow makes the patient susceptible to reentry and certain arrhythmias [7].
Additionally, using proton pump inhibitors (PPIs) in patients with GERD-induced esophagitis and paroxysmal AFib has improved sinus rhythm. Therefore, it has been proposed as a possible alternative to traditional anti-arrhythmic medications, further clarifying a possible connection between GERD and AFIB. [8].
Despite the vast amount of literature alluding to the association of GERD and AFib, research conducted regarding the association between GERD and other TAs is unclear and, most importantly, scarce. Regarding the second most common TA, there have been a few reported cases of patients developing atrial flutter status post-hiatal hernia development [9,10]. In a particular case, the patient opted for surgical hernia management with subsequent flutter resolution [10]. Regarding a less common TA, a study by Fuertes showed that SVT in newborns is associated with and may be caused by GERD [11].
This paper aims to clarify the relationship between GERD and the prevalence among other types of TAs. Furthermore, despite the similarities in the typical symptoms between both conditions, little is known about the outcomes linked with such a relationship. Therefore, we sought to find the association between GERD and TA compared to non-TA inpatient admissions.
Materials & Methods
We utilized the National Inpatient Sample (NIS) 2015 quarter 4 through 2019, a publicly available healthcare cost and utilization project database. Patients were identified using ICD-10 codes with a principal diagnosis of TA [atrial fibrillation, atrial flutter, paroxysmal tachycardia, AV reentrant tachycardia (AVRT), and supraventricular tachycardia (SVT)] and a secondary diagnosis of GERD; those aged 17 years and younger were excluded. Data are represented as weighted using an algorithm provided by NIS for accurate national estimates. Cohorts were weighted using an algorithm provided by the NIS, allowing for accurate national estimates. Multivariate regression models were adjusted for age, gender, race, Charlson Comorbidity Index (CCI), type of insurance, median household income based on zip code, hospital region, cocaine use, smoking, alcohol use, and cannabis use. Primary endpoints were the length of stay (LOS), hospital charges, and mortality.
Results
We identified 25,001,960 patients diagnosed with GERD, among which 478,835 (1.92%) had a diagnosis of TA. Patients 18 and older with GERD had higher odds of having TA compared to those without GERD [adjusted odds ratio (aOR) 1.18; p<0.001]. In addition, as seen in Table 1, patients presenting with TA and GERD were older compared to patients without TA (72 +/- 12 vs. 64.3 +/- 17.8), though both cohorts are more likely to be female (56.1% vs. 58.4%; p<0.001). Furthermore, there was no significant difference in CCI between patients with GERD and TA compared to the non-TA cohort (2.24 +/- 1.95 vs. 2.37 +/-2.21; p<0.001), as seen in Table 1.
Table 1: Baseline Characteristics of GERD Patients without and with Tachyarrhythmia.

Among patients presenting with GERD and TA, the most common cause of TA was atrial fibrillation (82.4%), followed by atrial flutter (10.2%) and SVT (7.3%); (p<0.001), as seen in Figure 1.
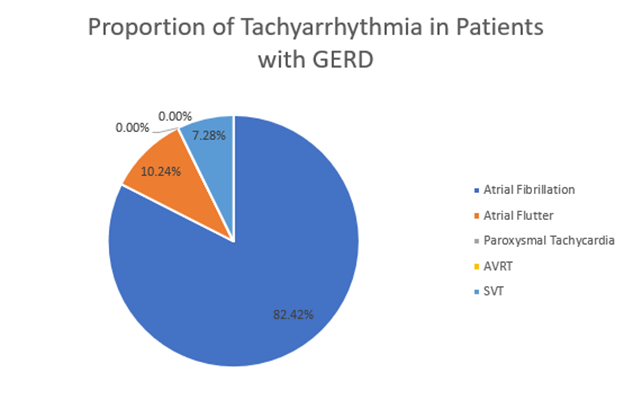
Figure 1: The proportion of Tachyarrhythmias in patients with GERD.
Surprisingly, patients with GERD and TA did not have higher mortality (aOR 0.34), LOS [adjusted mean difference (aMD) 1.45 days shorter), or hospital charges (aMD $14,463 less); all p<0.001.
Discussion
GERD and TAs are highly prevalent diseases that contribute to significant morbidity among the US population and a substantial portion of national healthcare costs. Through the analysis, it was found that both disorders may be associated with one another. Furthermore, the association is not limited to GERD and atrial fibrillation, as recorded in current literature. Still, this study has indicated a significant association between GERD and the presentation of various forms of TA, including atrial flutter and SVT.
Several studies have demonstrated the association between GERD and Afib [6-8,12]. However, our study has shown a correlation between Atrial Flutter, SVT, AFib, and GERD (p<0.001). In addition, multiple studies have suggested that lifestyle factors such as caffeine and alcohol intake may exacerbate GERD and several TAs, including AFib and PSVT [13]. Therefore, since ingestion of caffeine or alcohol may affect TAs other than AFib and GERD, this may further explain the relationship between GERD and several forms of TA.
Significant variability in outcomes and demographic factors was observed among the GERD patients between those with TA and those without TA. Therefore, factors including CCI, sex, and race were analyzed to understand the relationship between GERD and TA.
Out of all patients presenting with GERD, patients presenting with any subtype of TA were significantly older, at an average age of 72, than those not presenting with any TA, at an average age of 64 (p<0.0001). Furthermore, several types of TAs, including atrial fibrillation and atrial flutter, composed 82.42% and 10.24% of the studied patients, are age-related arrhythmias and tend to manifest in the eighth decade of life [14,15].
Additionally, a more significant proportion of females were found among all GERD patients, in both those presenting with and without TAs. This most likely occurred because, in those older than 65, the average age of our study population, GERD presents more often in females than males [16]. Furthermore, a significant increase in prevalence among females was detected in those offering without TAs (p<0.0001), likely due to a known two-fold increase in the majority of atrial fibrillation, the most common TA in the study among men compared to that of women [17].
Moreover, variabilities between races were also observed. For example, in all GERD patients included in the study, a higher proportion of whites were likelier to have experienced at least one TA than non-whites (p<0.0001).
Of those presenting with GERD and TA, 84.6% were white, and 15.4% were non-whites (Black, Hispanic, Asian or Pacific Islander, Native American, and others). As opposed to those presenting with GERD and without TA, 76.1% were white, and 23.9% were non-white, showing a higher proportion of whites with GERD who experienced a TA episode than those who did not experience a TA. In comparison, a higher proportion of non-whites with GERD were less likely to experience a TA episode than those who experienced a TA. Despite the general association that exists between GERD and TAs, non-whites may have distrust in the healthcare system [18], may not seek out medical care due to decreased health literacy [19], or may have less access to healthcare resources than their white counterparts [20]. Therefore, they may be less likely to seek hospitalization for GERD and hence would not be able to simultaneously be diagnosed with GERD and TA. Therefore, the prevalence of TAs in GERD patients amongst the white population would be higher because whites are more likely to seek hospitalization [21]. However, these disparities may be linked to a decrease in sample size and statistical power, as there is a higher sample number (n = 24,523,125 > n = 478,835) in the group without tachyarrhythmias.
Despite the additional morbidity of having a TA and GERD, no significant difference was found between CCIs, or the ten-year mortality rates, of both TA and non-TA groups (p<0.0001). Furthermore, it was confirmed by comparing clinical outcomes between those with and without TAs, such as LOS, hospital charges, and mortality. Additionally, the CCI for the TA group, 2.2, was comparable to that of the non-TA group, at 2.4, thereby eliminating the possibility of other comorbidities serving as confounding factors to attributable differences between those with and without TAs among GERD patients. Therefore, GERD is seemingly the most attributable factor to a patient's likelihood of developing a TA.
Despite the study's integrity, significance, and potential impact on the future treatment of patients presenting with GERD and TAs, several limitations should be considered. Firstly, as more research regarding the association between both conditions is being explored, the standard treatment for GERD, or proton pump inhibitors (PPIs), is associated with significantly greater odds of developing focal TAs due to the presence of H+/K+ ATPase in myocardial tissue [22]. For this reason, the patients included in the study may be developing TAs due to the PPI medications rather than due to the condition of GERD itself. In addition, the disparities in racial outcomes may be linked to a decrease in sample size and statistical power, as a small amount of TA patients are included in the sample with a higher sample number (n = 24,523,125 > n = 478,835) in the group without tachyarrhythmias. However, these distributions resulted from the complex nature of obtaining patients and database extraction for the study. Lastly, due to the novelty of our research, the relationship between GERD and TA is merely an association, as the causation is yet to be determined. Therefore, more randomized controlled trials (RCTs) need to be conducted to strengthen the correlation between the two pathologies.
Conclusion
The association of TA in patients with GERD is often clinically seen but lacks a clear explanation. Our study observed that patients with GERD had higher odds of having TA. However, such arrhythmias did not increase mortality, LOS, or hospital charges. There lies a need for further exploration to identify GERD as an underlying etiology for such common arrhythmias and treat it appropriately to minimize TA-related complications.
Funding/Support: None
Statement: None of the authors have any proprietary interests.
References
- Haghjoo M. Chapter-13: Tachyarrhythmias. Practical Cardiology (2nd Ed), Elsevier, 2022: 257-277. doi: 10.1016/B978-0-323-80915-3.00016-8
- Pollack Jr. CV, Cantor RM, Blank JF. Tachyarrhythmias. Differential Diagnosis of Cardiopulmonary Disease. Springer, Cham, 2019: 1013-1035. doi: 10.1007/978-3-319-63895-9_68
- Khurshid S, Choi SH, Weng L-C, Wang EY, Trinquart L, Benjamin EJ, et al. Frequency of Cardiac Rhythm Abnormalities in a Half Million Adults. Circ Arrhythm Electrophysiol, 2018; 11(7): e006273 doi: 10.1161/CIRCEP.118.006273
- Antunes C, Aleem A, Curtis SA. Gastroesophageal reflux disease. StatPearls [Internet] StatPearls Publishing; 2021.
- Chen J, Brady P. Gastroesophageal Reflux Disease. Gastroenterol Nurs, 2019: 42(1); 20-28. doi: 10.1097/SGA.0000000000000359
- Roman C, Bruley des Varannes S, Muresan L, Picos A, Dumitrascu DL. Atrial fibrillation in patients with gastroesophageal reflux disease: a comprehensive review. World J Gastroenterol, 2014; 20(28): 9592-9599. doi: 10.3748/wjg.v20.i28.9592
- Velagapudi P, Turagam MK, Leal MA, Kocheril AG. Atrial fibrillation and acid reflux disease. Clin Cardiol, 2012; 35(3): 180-186. doi:10.1002/clc.21969
- Stöllberger C, Finsterer J. Treatment of esophagitis/vagitis-induced paroxysmal atrial fibrillation by proton-pump inhibitors. J Gastroenterol, 2003; 38(11): 1109. doi: 10.1007/s00535-003-1216-6
- Bengaluru J, Manju, WM, Hussam A. A Large Hiatal Hernia Presenting with Symptomatic Atrial Flutter and Echocardiographic Left Atrial Mass, CHEST, 144(4): 150A. https://doi.org/10.1378/chest.1705305
- Patel A, Shah R, Nadavaram S, Aggarwal A. Hiatal hernia squeezing the heart to flutter. The American Journal of Emergency Medicine, 32(4): 392.e1-392.e2. https://doi.org/10.1016/j.ajem.2013.10.024
- Fuertes Á, Alshweki A, Pérez-Muñuzuri A, Couce ML. Supraventricular tachycardia in newborns and its association with gastroesophageal reflux disease. Anales de Pediatria, 2017; 87(4): 206-210. doi: 10.1016/j.anpedi.2016.10.006
- Kunz JS, Hemann B, Edwin Atwood J, Jackson J, Wu T, Hamm C. Is there a link between gastroesophageal reflux disease and atrial fibrillation? Clin Cardiol, 2009; 32(10): 584-587. doi: 10.1002/clc.20660.
- Liang Y, et al. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ, 2012; 184(16): E857-E866.
- Granada J, Uribe W, Chyou PH, Maassen K, Vierkant R, Smith PN, et al. Incidence and predictors of atrial flutter in the general population. J Am Coll Cardiol, 2000; 36(7): 2242-2246. doi: 10.1016/s0735-1097(00)00982-7.
- Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med, 1995; 155(5): 469-473.
- Fakhre H. Gender is a risk factor in patients with gastroesophageal reflux disease. Med J Islam Repub Iran, 2017; 31: 58. doi: 10.14196/mjiri.31.58.
- Mayor S. Men develop atrial fibrillation 10 years earlier than women, finds study BMJ, 2017; 359: j4802 doi: 10.1136/bmj.j4802
- Krakauer EL, Crenner C, Fox K. Barriers to optimum end-of-life care for minority patients. J Am Geriatr Soc, 2002; 50(1): 182-90. doi: 10.1046/j.1532-5415.2002.50027.x.
- Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the "newest vital sign" ease of use and correlates. J Am Board Fam Med, 2010; 23(2): 195-203. doi: 10.3122/jabfm.2010.02.070278.
- Vines AI, Godley PA. The challenges of eliminating racial and ethnic health disparities: inescapable realities? Perplexing science? Ineffective policy? N C Med J, 2004; 65(6): 341-349.
- Jia P, Xierali IM. Disparities in Patterns of Health Care Travel Among Inpatients Diagnosed with Congestive Heart Failure, Florida, 2011. Prev Chronic Dis, 2015; 12: E150. doi: 10.5888/pcd12.150079.
- Marcus GM, Smith LM, Scheinman MM, et al. Proton pump inhibitors are associated with focal arrhythmias. The Journal of Innovations in Cardiac Rhythm Management, 2010; 1(4): 85-89. doi: 10.19102/icrm.2010.011206

