Post-Traumatic Diaphragmatic Hernia Revealed by an Occlusive Syndrome
Mohamed Oussama Bahri1,2,*, Abdeslam Bouassria1,2, Hicham El Bouhaddouti1,2, Ouadii Mouaqit1,2, El Bachir Benjelloun1,2, Abdelmalek Ousadden1,2 and Khalid Ait Taleb1,2
1School of medicine and pharmacy of Fez, Sidi Mohammed Ben Abdellah University, Morocco
2Department of surgery, University Hospital Hassan II, Morocco
Received Date: 14/04/2023; Published Date: 25/07/2023
*Corresponding author: Mohamed Oussama Bahri, School of Medicine and Pharmacy of Fez, Sidi Mohammed Ben Abdellah University, Department of Surgery, University Hospital Hassan II, Fez, Morocco
Summary
Post-traumatic diaphragmatic hernia is a particular lesion in polytrauma patients that may go unnoticed. The diagnosis is then made on the occasion of a complication [1].
Post-traumatic diaphragmatic hernia should be systematically diagnosed.
We report the case of a young 37-year-old patient victim of a public road accident presenting a post traumatic diaphragmatic hernia revealed by the association of vomiting with an acute occlusive syndrome, chest pain and acute respiratory distress.
Keywords: Diaphragmatic hernia; Abdominal trauma; Occlusion; General surgery
Introduction
Post-traumatic diaphragmatic hernia is a particular lesion in polytrauma patients that may go unnoticed. The diagnosis is made when a complication occurs [1]. The left diaphragmatic dome is the most frequently affected and can quickly become life-threatening.
Post-traumatic diaphragmatic hernia should be systematically investigated by a thoracic X-ray or a thoraco-abdominal CT scan in the case of any abdominal trauma with hyper pressure. Its treatment is surgical.
Patient and Observation
This is a young patient, 37 years old, with no notable pathological history.
Admitted to the emergency room of our training 4 days after the patient was victim of a public road accident with ejection of the car.
The clinical examination on admission revealed a tachycardia patient at 110 beats/min with hypotension at 100/70 mmhg, FR: at 26 cycles/min and temperature at 37°C.
Abdominal examination showed abdominal tenderness and some episodes of vomiting with an acute occlusive syndrome chest pain and acute respiratory distress.
After initial conditioning:
2VVP + vascular filling + with intravenous injections of proton inhibitors. SNG, SU
A biological check-up on admission showed a hyperleukocytosis of 11,000 with a predominance of PNN and a CRP of 141 with a normal ionogram, a prothrombin rate of 100% and a hemoglobin of 11.5
A thoracic-abdominal-pelvic CT scan (Figure 1,2):
- Focus of contusion and alveolar hemorrhage of the left pulmonary hemichampus and right lower lobe associated with a small bulla of left lower lobar pneumatocele, Pneumomediastinum associated with a large emphysema dissecting the soft parts of the left chest wall, fusing upwards towards the homolateral axillary region, Hemomediastinum opposite a double fracture line of the sternal manibrium, without significant displacement
- Post-traumatic left diaphragmatic hernia, involving a portion of the greater gastric curve intrathoracically
The patient went to the operating room: after a median laparotomy, the exploration showed a diaphragmatic defect of 3 cm containing the gastric greater curvature and a part of the transverse colon
The procedure consisted of lowering the stomach and colon, which were viable without signs of suffering, and then suturing the diaphragm with a non-absorbable thread in a separate stitch (Figure 3,4).
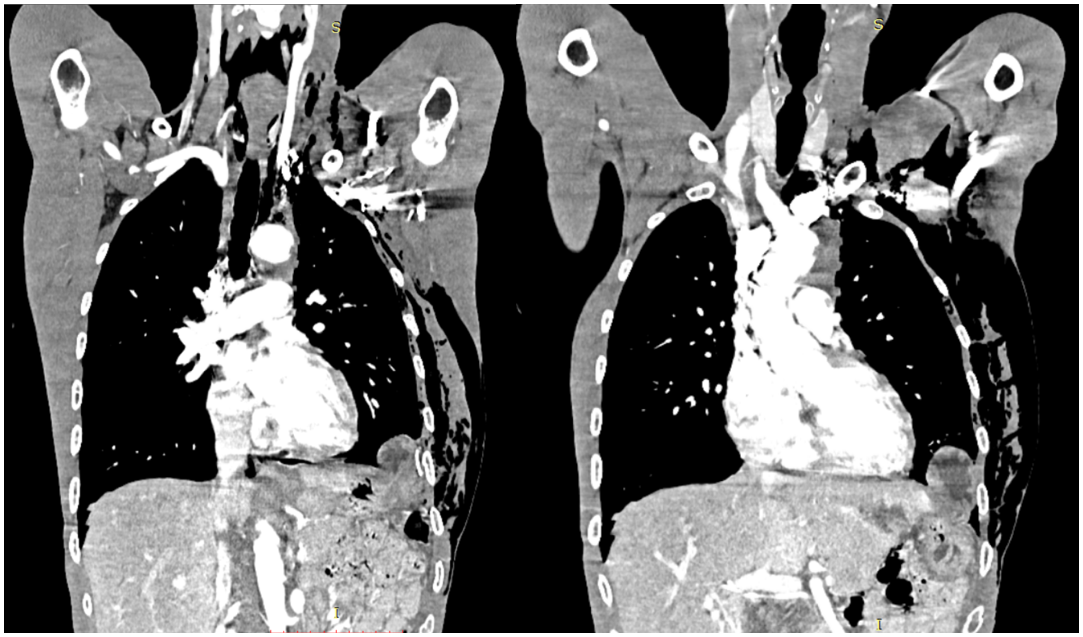
Figure 1: Coronal reconstruction of injected thoracoabdominal CT scan showing the assenions of the stomach and colon.
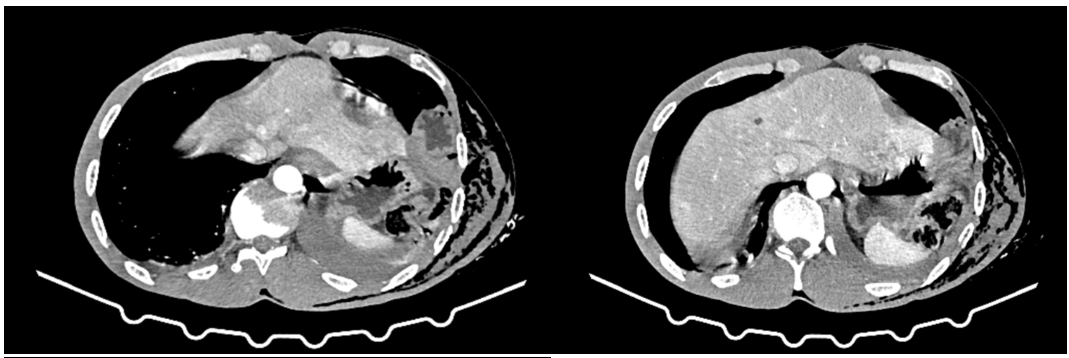
Figure 2: Axial slices of the thoracoabdominal CT injector.

Figure 3: Intraoperative image showing the diaphragm wound.
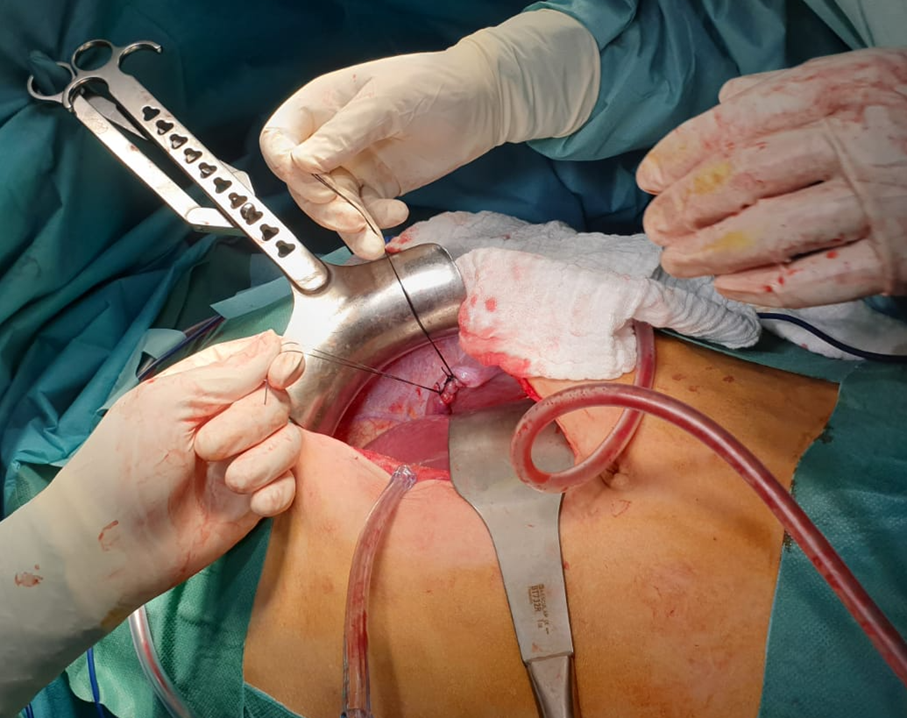
Figure 4: Image showing the suture of the diaphragmatic wound.
Discussion
Posttraumatic diaphragmatic hernias correspond to a muscular breach of the diaphragmatic dome that may be complicated by an intrathoracic exit of the surrounding abdominal viscera. They often testify to the severitý of the trauma, but remain mostly among the most misunderstood lesions [1]. The etiologies of diaphragmatic hernias are dominated by polytrauma and thoracoabdominal wounds; they rarely involve laborious delivery, crush injury, or postoperative hernia [2-5].
Anatomically, the site is, in 70 to 90% of cases, the left diaphragmatic dome, taking into account the protective role of the liver on the right. The contents of the hernia are variable, the most frequent organs found in these hernias are, in decreasing order of frequency: the stomach (31.8%), the colon (27.2%), the omentum (15.9%), the small intestine (13.6%), the spleen (6.8%) and the liver (4.5%) [7].
From a diagnostic point of view, the vital emergency due to the polytrauma often delays the diagnosis and, in half of the cases, HD is ignored [7], which is the case of our patient who had suffered a very serious abdominothoracic trauma 4 days ago following a road accident. Thus, the revelation can be made late, on the occasion of a complication such as a strangulation or an occlusion and the major risk in this case, is the perforation of the herniated hollow viscera in intrathoracic.
Clinically, the association of vomiting with acute occlusive syndrome, chest pain and acute respiratory distress [4,6]. In our case, the patient had initially presented with vomiting.
The paraclinical work-up was based on a chest X-ray, which showed a hydropneumothorax with a digestive loop image in the intrathoracic region [8]. However, it seems that the spiral CT scan allowing transverse and coronal sections, as well as three-dimensional images, remains the best examination in this context. This technique reveals the hernia, but also shows the complications induced on the herniated organs [9].
Therapeutically, laparotomy is the most frequently used approach. It allows reduction of the hernia. Repair of the diaphragm must be performed by separate stitches with non-resorbable thread [3]. However, in the case of a major defect of the diaphragmatic dome, the use of prosthetic plasty may be useful to reinforce the raphe. However, since non-absorbable prostheses are contraindicated in a septic context, it is preferable to use absorbable prostheses [6].
The postoperative course is marked mainly by the development of septic complications. Empyema is the most frequent complication and may require secondary decortication [11]. Mortality remains high despite immediate surgical management. It can reach 25 to 66% [10]. In our case, no complication was noted and the evolution was good with, especially, the resumption of a normal respiratory dynamics.
From a preventive point of view, the best way to make an early diagnosis of diaphragmatic hernia and thus avoid its complications is to systematically evoke it in case of violent thoraco-abdominal trauma, since it may go unnoticed in front of the vital emergency and because of the poor clinical picture.
Conclusion
The occurrence of a diaphragmatic hernia should be routinely in mind in case of violent closed thoracoabdominal trauma or in case of basithoracic wound, strangulation of a diaphragmatic hernia should be thought of especially in case of a history of thoracoabdominal trauma.
Conflicts of Interest: The authors declare no conflicts of interest.
Author Contributions: All authors have read and approved the final version of the manuscript.
References
- Slim K. Ruptures et plaies du diaphragme. J Chir, 1999; 136: 67.
- Hammoudi D, Bouderka MA, Benissa N, Harti A. Diaphragmatic rupture during labour. Int J Obstet Anesth, 2004; 13: 284-286.
- Lenriot JP, Paquet JC, Estephan H, Selcer D. Traitement chirurgical des ruptures traumatiques du diaphragmatique. EMC techniques chirurgicales. App Digest, 1994; 10: 40-240.
- Ramdass MJ, Kamal S, Paice A, Andrews B. Traumatic diaphragmatic herniation presenting as a delayed tension fecopneumothorax. Emerg Med J, 2006; 23: e54.
- Markogiannakis H, Theodorou D, Tzertzemelis D, Dardamanis D, Toutouzas KG, Misthos P, et al. Fecopneumothorax: a rare complication of oesophagectomy. Ann Thorac Surg, 2007; 84: 651-652.
- Jarry J, Razafindratsira T, Lepront D, Pallas G, Eggenspieler P, Dastes FD. Une complication rare des hernies diaphrag- matiques traumatiques: la pleurésie stercorale. Ann Chir, 2006; 131: 48-50.
- Nursal TZ, Ugurlu M, Kologlu M, Hamaloglu E. Traumatic dia- phragmatic hernias: a report of 26 cases. Hernia, 2001; 5: 25-29.
- Cruz CJ, Minagi H. Large-bowel obstruction resulting from trau- matic diaphragmatic hernia: imaging findings in four cases. AJR Am J Roentgenol, 1994; 162: 843-845.
- Eren S, Ciris F. Diaphragmatic hernia: diagnostic approaches with review of the literature. Eur J Radiol, 2005; 54: 448-459.
- Grimes OF. Traumatic injuries of the diaphragm. Diaphragmatic hernia. Am J Surg, 1974; 128: 175-181.
- Vermillion JM, Wilson EB, Smith RW. Traumatic diaphragmatic hernia presenting as a tension fecopneumothorax. Hernia, 2001; 5: 158-160.

