Complications of Percutaneous Endoscopic Gastrostomy Placement
Shaniah Holder1,*, Gabrielle Unbehaun2, Marie Wisa Beauge2, Sarah Miraaj-Raza3, Jahanvi Joshi3 and Frederick Tiesenga4
1Department of Medicine, American University of Barbados School of Medicine, Barbados
2Department of Medicine, Saint George’s University School of Medicine, Grenada
3Department of Medicine, Saint James School of Medicine, Anguilla4Department of Surgery, Community First Hospital
Received Date: 16/03/2023; Published Date: 05/06/2023
*Corresponding author: Shaniah Holder, 1Department of Medicine, American University of Barbados School of Medicine, Barbados
Abstract
A Percutaneous Endoscopic Gastrostomy (PEG) tube, often referred to as a G-tube, is an instrument that is placed directly through the abdominal wall to access the stomach. It is a necessary procedure employed for various reasons, from achieving enteral nutrition in individuals who suffer from dysphagia and malnutrition to maintaining nutrition in a comatose patient. Though most complications are minor, the possibility of major complications exists. Due to the cavernous variation in rates of complications, it is an essential subject to appreciate when assessing a patient for PEG tube placement or malfunction. We present a case of a 62-year-old male who presented to the emergency department for a malfunctioning PEG tube with multiple complications such as cellulitis, intraabdominal injury, and leakage of gastric contents. This report aims to explore these complications, their clinical presentation, the diagnostic approach, and surgical management.
Keywords: Percutaneous Endoscopic Gastrostomy tube; Wound Infection; Intrabdominal Injury Intussusception; Peristomal Leakage
Introduction
Critically ill patients or healthy individuals undergoing major surgeries are the most at risk to develop malnutrition with a prevalence of 50 percent [1,2]. In the presence of malnutrition, there is an increased catabolic state leading to loss of fat, muscle, and eventually, bone and viscera mass [2]. In such a state, homeostatic responses are impaired thus exposing the body to negative consequences like infections, poor wound healing, increased risk of decubitus ulcers, bacterial overgrowth in the Gastrointestinal (GI) tract, and excess nutrient loss through the stool [2].
Nutritional interventions such as oral supplementation, enteral (tube) feeding, or parenteral (intravenous) feeding are started when it becomes evident that the patient will not be able to maintain adequate nutrition [3]. In patients with functional GI systems, enteral nutrition is preferred over parenteral due to the risks associated with the intravenous route, higher cost, and the inability of parenteral nutrition to provide GI stimulation which compromises the gut defense barrier [5].
Enteral feeding may be delivered in a gastric or postpyloric fashion, but gastric is the most common type [4]. They can be placed endoscopically, radiographically, or surgically [6]. Percutaneous endoscopic gastrostomy (PEG), first introduced in 1980 by doctors Ponsky and Gauderer, is the preferred type of tube due to its minimally invasive method of access, low cost, and decreased risk of bacteremia [4-6]. Some complications related to PEG are infections, bleeding, peristomal leakage, and ulceration [6].
In this case report, we present a 62-year-old patient who came to the Emergency Department (ED) with multiple complications of the PEG tube that was placed years prior.
Case Presentation
We present a 62- year-old male with a past medical history significant for substance use disorder and surgical history remarkable for Tracheostomy and PEG tube placement. He presented to the ED for a malfunctioning PEG tube. The patient was cachectic in appearance. On physical exam, there was a large open stoma with leakage of gastric contents around the tube and erythema of the skin concerning for cellulitis. Laboratory tests were significant for leukocytosis with a White Blood Cell (WBC) count of 21,000 per µL therefore the patient was placed on prophylactic cefepime. (Figure 1) below shows leakage of gastric contents around the PEG tube.

Figure 1: PEG tube visualized with leakage of contents through the stoma and surrounding erythema.
A Computed Tomography (CT) Scan of the Abdomen and Pelvis with intravenous (IV) contrast was conducted and showed the PEG tube in a normal position with the proximal end in the stomach and the distal end in the small bowel. Conservative treatment with Cefepime and Vancomycin in addition to local skin care with topical zinc oxide was utilized, however, the patient’s condition continued to deteriorate with his WBC count increasing to 24,000 per µL. Due to these acute findings, it was decided to take down the gastrocutaneous fistula and replace the gastrojejunostomy tube.
During the procedure, the site of the old PEG tube was visualized and the gastrocutaneous fistula was transected with an Endo-GIA™ (Medtronic, Minneapolis MN) device. The protruding gastric remnant was excised and the area was repaired. At this time, a large anteriorly perforated gastric ulcer at the level of the antrum was found. The patient needed a new PEG tube and the decision was made to use the large gastric ulcer as the new placement site. The stomach was pexed to the anterior abdominal wall and antibiotic irrigation was utilized. There were no surgical complications and the patient subsequently began tube feeds. Pathology of the gastric tissue around the ulcer showed extensive inflammation and necrosis without Helicobacter pylori. (Figure 2, 3) below show the necrotic tissue with cell sloughing.

Figure 2: Gastric tissue showing cellular inflammation on microscopy.
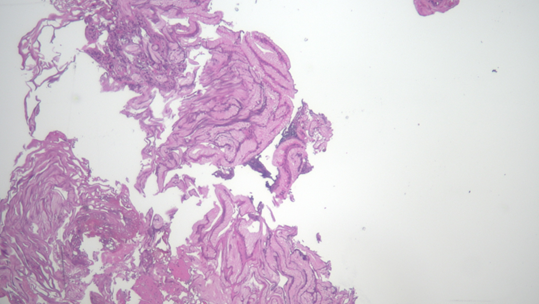
Figure 3: Cellular necrosis with degeneration of tissue visualized.
Blood cultures were positive for Staphylococcus haemolyticus and the abdominal wound cultures grew Candida albicans. Nine days postoperative, his leukocytosis began to resolve and the patient was tolerating the PEG tube feeds with no leakage reported. An additional abdominal CT scan was conducted to follow up on some mild abdominal pain reported by the patient and found a small bowel intussusception. (Figure 4) below shows the intussusception.

Figure 4: Classic “Target Sign” of the Small Bowel indicating Intussusception.
Due to his history of recent surgery, lack of severe symptoms, and presence of Acute Kidney Injury (AKI), it was decided by the primary team that a barium enema could not be conducted and surgical reduction of the intussusception would not improve his clinical outcome so those were deferred at the time. In the following weeks, the patient’s abdominal pain resolved and he continued tolerating feedings through the PEG tube, therefore after medical optimization, the patient was transferred to a skilled nursing facility to continue care.
Discussion
PEG is a minimally invasive option for providing enteral nutrition. Indications for PEG placement include patients with moderate to severe nutritional deficiency requiring more than 30 days of feeding, patients requiring gastric decompression, and the management of gastric volvulus [5,6]. Since its introduction, the PEG has become the preferred method for providing long-term enteral nutritional support and is associated with a major complication rate between 1-4% and a mortality rate of approximately 1% [5-8]. Minor complications are relatively common with 35.6% of patients experiencing at least one complication and 6.6% of patients experiencing three complications within one year of PEG placement [7]. PEG tube complications are predominantly classified as minor or major. Minor complications include wound infection and stoma leakage [5-7]. Major complications can include intussusception and internal organ injury [5-7].
Wound Infection
As seen in this patient, local wound infection is one of the most common complications occurring in 4-30% of patients [8,9]. Patients with diabetes mellitus, active malignancy, chronic corticosteroid use, previous radiation, or severe nutritional compromise are at increased risk [8,9]. These infections are often polybacterial with Pseudomonas aeruginosa, Candida albicans, Staphylococcus aureus, and Escherichia coli being the most common causative organisms [9,10]. Signs of infection include stomal erythema, purulent discharge, fever, and chills [8,9]. Initial management should be determined based on the severity of the infection with topical antibiotics for mild cases and broad-spectrum antibiotics for moderate to severe infections [11]. Rarely, PEG tube removal may be required if the infection is unresponsive to treatment [11]. Pre-procedure skin decontamination and prophylactic antibiotics can greatly reduce the risk of infection [11].
Peristomal Leakage
Peristomal leakage occurs in approximately 1-10% of patients [6,11]. Excessive side torsion, gastric hypersecretion, infection, slow wound healing, and excessive cleaning can increase its risk [9,11]. Signs of leakage can be similar to wound site infection and include stomal erythema and peristomal skin maceration, but peritoneal irritation and rebound tenderness can help differentiate the diagnosis of these complications [9,11]. Any assessment of peristomal leakage should include a detailed evaluation of the PEG tube fit and determination of leakage composition [11]. Management should include protection of the surrounding skin and initiation of a proton pump inhibitor [9,11]. If the leakage cannot be resolved with these measures, the PEG should be removed and replaced at an alternate site [11].
Intra-Abdominal Injury
Iatrogenic intra-abdominal organ injury, including perforation of the stomach, spleen, liver, and large and small bowel, is a rare complication associated with the PEG tube placement. The incidence of this complication is reported to be between 0.5-1.8% and is typically due to malposition of the PEG [5,8,12]. Perforation occurs more often in the elderly and the very young due to the laxity of the colonic mesentery [5]. Signs of these injuries can include diarrhea, fecal material in the PEG tube, feculent vomiting, altered mental status, or pneumoperitoneum [5,12]. Diagnosis is challenging and typically requires the use of a CT with contrast revealing evidence of leakage [5,12]. Repair of this complication is considered a surgical emergency [5].
Intussusception
Postoperative intussusception is an exceptionally rare and serious complication of PEG placement. The incidence of intussusception has been reported to be around 0.38% occurring between 10-69 days after surgery [13]. General symptoms include crampy abdominal pain, bloody mucus-containing stool, diarrhea, and bloating [14,15]. Due to the generalized symptoms, diagnosis can be challenging. CT is the most sensitive diagnostic tool which can provide additional information on the anatomic details such as the lead point and the possibility of self-resolution [14-15]. An intussusception may appear as a sausage-shaped mass or as the classical “target sign”, as seen in the case presented [15]. Management is dependent on the location, size, associated bowel viability, and stability of the patient [15]. Some cases may self-resolve and require only supportive treatment with pain medications, IV fluids, and antiemetics [15]. However, most will require surgical correction.
Conclusion
The PEG tube is an essential conduit to achieving adequate nutrition in countless patients. Clinical applications include but are not limited to, persistent dysphagia, hydration, medication administration, and patients requiring gastric decompression. The PEG tube’s enteral mode is superior to others due to its cost efficiency, success rate, and low procedural mortality rates. However, many complications can arise from this device such as infection, leakage, intrabdominal injury, and intussusception, all of which occurred in this one patient. It is important for physicians to understand the etiologies of these complications for prompt diagnostic and therapeutic management. Close postoperative follow-up should also be implemented as a preventative measure in persons with PEG tube placement.
Author Contributions
Shaniah Holder: Concept and Design of study, Acquisition of data, drafting article, revising article. Guarantor Author
Gabrielle Unbehaun: Concept and Design of study, drafting article intellectual content, revising article
Marie Wisa Beauge: Acquisition of data, drafting article, revising article
Sarah Miraaj-Raza: Acquisition of data, drafting article, revising article
Jahanvi Joshi: drafting article, revising article
Frederick Tiesenga: Final Approval, Intellectual Content, revising article
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case
Competing Interests: None
Grant Information: None
References
- McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ, 1994; 308(6934): 945-948.
- Elwyn DH, Bryan-Brown CW, Shoemaker WC. Nutritional aspects of body water dislocations in postoperative and depleted patients. Ann Surg, 1975; 182(1): 76-85.
- Klein S, Kinney J, Jeejeebhoy K, Alpers D, Hellerstein M, Murray M, et al. Nutrition support in clinical practice: review of published data and recommendations for future research directions. Clin Nutr, 1997; 16(4): 193-218.
- ASPEN Board of Directors, Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr, 2002; 26(1 suppl): 1-138.
- Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol, 2014; 20(24): 7739-7751.
- Larson DE, Burton DD, Schroeder KW, DiMagno EP. Percutaneous endoscopic gastrostomy. Indications, success, complications, and mortality in 314 consecutive patients. Gastroenterology, 1987; 93(1): 48-52.
- Boylan C, Barret D, Li V, Merrick S, Steed H. Longitudinal complications associated with PEG: Rate and severity of 30-day and 1-year complications experienced by patients after primary PEG insertion. Clinical Nutrition ESPEN, 2021; 43: 514-521.
- Ghevariya V, Paleti V, Momeni M, Krishnaiah M, Anand S. Complications Associated with Percutaneous Endoscopic Gastrostomy Tubes. Annals of Long-Term Care, 2009.
- Potack JZ, Chokhavatia S. Complications of and controversies associated with percutaneous endoscopic gastrostomy: report of a case and literature review. Medscape J Med, 2008; 10(6): 142.
- Krishna S, Singh S, Dinesh KR, Kp R, Siyad I, Karim S. Percutaneous Endoscopic Gastrostomy (PEG) site infections: a clinical and microbiological study from university teaching hospital, India. J Infect Prev, 2015; 16(3): 113-116.
- Boeykens K, Duysburgh I, Verlinden W. Prevention and management of minor complications in percutaneous endoscopic gastrostomyBMJ Open Gastroenterology, 2022; 9: e000975.
- Boeykens K, Duysburgh I. Prevention and management of major complications in percutaneous endoscopic gastrostomy BMJ Open Gastroenterology, 2021; 8: e000628.
- Hu Liangshuo, Yin Guozhi, Zhang Dong, Geng Zhimin, Bai Jigang. Tube feeding associated postoperative intussusceptions: A single center case series study. Medicine, 2019; 98(44): 17783.
- Govednik C, Cover J, Regner JL. Preventing retrograde jejunoduodenogastric intussusception as a complication of a long-term indwelling gastrostomy tube. Proc (Bayl Univ Med Cent), 2015; 28(1): 34-37.
- Brill A, Lopez RA. Intussusception in Adults. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2022.

