A Rare Case of Infant Circumcision Complicated with Life-Threatening Klebsiella Pneumoniae Infection
Ayesha Yasir1, Adnan Mirza2, Rafia Naeem3, Waqar Ahmed1, Mohammad Aadil Qamar4,*
1Fellow, Infectious disease, Aga Khan University, Pakistan
2Assistant Professor, Neonatal medicine, Department of Pediatrics, Aga Khan University Hospital, Pakistan
3Medical College, Karachi Medical and Dental College, Pakistan
4Medical College, Ziauddin University, Pakistan
Received Date: 26/02/2023; Published Date: 04/05/2023
*Corresponding author: Mohammad Aadil Qamar, Medical College, Ziauddin University, 4/B, Shahrah-e-Ghalib Road, Block 6, Clifton, Karachi 75600, Sindh, Pakistan
Abstract
Circumcision is a common surgical procedure associated with complications due to untrained circumcisers, lack of sterility during the procedure, and the advanced age of the patient to mention a few. The most common complication reported is sepsis. We present a rare case of an 8-day-old infant who developed a life-threatening Klebsiella Pneumoniae infection after circumcision. He was born at 37+2 weeks of gestation via an emergency caesarian section. He underwent circumcision on the 6th day of his life, and developed scrotal swelling, tachycardia, hypoperfusion, and fever on the 8th day of life. He was referred to our hospital for further management. An intravenous (IV) line was maintained along with meropenem and vancomycin. He developed right buttock and ankle swelling during his stay in the Intensive Care Unit (ICU). Blood, urine, and pus cultures were positive for Klebsiella Pneumoniae which was sensitive to meropenem. Subsequently, it was decided to continue meropenem and vancomycin for 6 weeks. At 3 months of age, the patient presented to the emergency department due to fever and inability to move his left leg for 3 days. Meropenem, colistin, and vancomycin were given. He was discharged home upon stabilization. On a follow-up visit, the child was healthy and thriving with no signs of infection. Our data demonstrated that fatal complications could occur because of circumcision. These complications can be prevented early on by taking appropriate measures. The main purpose of this paper is to discuss the possible ways to avoid complications following pediatric circumcision.
Keywords: Circumcision; Complications; Klebsiella Pneumonia; Infection; Neonate; Outcome
Abbreviations: IV: Intravenous; ICU: Intensive Care Unit; APGAR: Appearance; Pulse; Grimace; Activity; and Respiration; BCG: Bacille Calmette-Guerin; AP: Anteroposterior; NK: Natural Killer; MRI: Magnetic Resonance Imaging; CC: Cubic Centimeters; HSV: Herpes Simplex Virus; TB: Tuberculosis; WHO: World Health Organization; SOPs: Standard Operating Procedures.
Introduction
Circumcision is a common surgical procedure practiced in many cultures as a part of their ritual tradition. It is estimated that 1.2 million newborn males are circumcised in the USA annually [1]. The medical benefits that support this practice include the prevention of phimosis, balanitis, paraphimosis, and a decrease in the risk of cancer of the penis, and urinary tract infections among infants [1]. The overall rate of complication is 0.2% to 5% [2]. Complications arise when it is performed by an inexperienced individual [3]. Moreover, the age of a child also plays an important role. Children above 2 years of age are at increased risk of complications [4]. The highest frequency complications are reported in developing countries including Pakistan [5]. In this article, we describe a case of Klebsiella pneumoniae presented as multiple abscesses associated with ritual circumcision.
Case Presentation
A 2.2 kg male infant was born at 37+2 weeks of gestational age by an emergency cesarean section due to breech presentation and maternal complications. Mother was a known case of hypothyroidism and pregnancy-induced hypertension, both were well-controlled with medication. She received appropriate antenatal care, and all her scans were normal. Neonate cried immediately after birth. His Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) scores were 8 and 9 in the 1st and 5th minute, respectively. The height and head circumference were appropriate for the gestational age. His head-to-toe examination and systemic examination were unremarkable. He received the recommended Bacille Calmette-Guerin (BCG) and polio vaccines and was discharged home after thyroid and hearing assessments.
The neonate underwent circumcision in a private hospital on the sixth day of his life. After two days he developed scrotal swelling and fever. He was referred to our tertiary care private institution for further management. Upon presentation, the child had a fever, tachycardia, decreased pulse rate, and hypoperfusion. The right-sided scrotum was red, warm, and tender to the touch. An IV line was maintained, and normal saline boluses were given. After sending a septic workup (blood culture test, cerebrospinal fluid, urine culture, and sensitivity test), meropenem and vancomycin were started at a renal-adjusted dose due to raised creatinine levels. Ultrasound scrotum reported on a right-sided scrotal pyocele (Figure 1). Pediatric surgery was taken on board and 5ml of frank pus was drained and cultures were sent. His ultrasound kidney was planned due to raised creatinine which showed a horseshoe kidney and mild dilation of the left-sided pelvicalyceal system with an AP diameter of the left renal pelvis of 5.4 mm. Nephrology was taken on board and a repeat kidney ultrasound scan at the time of discharge was suggested.
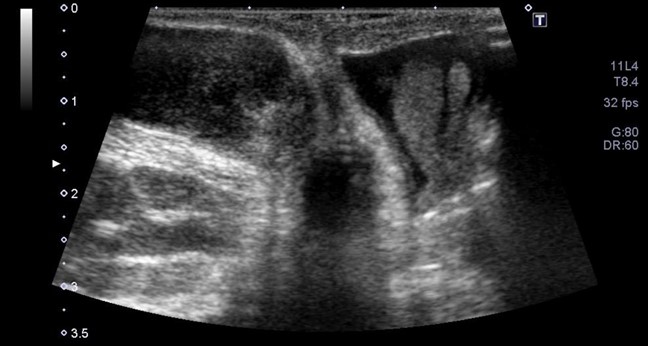
Figure 1. Ultrasound of Right scrotum showing scrotal swelling, complex fluid collection in the right hemiscrotum pushing the testicle peripherally and not tracking above the scrotum.
During their stay in the Neonatal ICU, he developed right buttock swelling, which was reddish, tender, and gradually increasing in size. The swelling was also drained. Meanwhile, his blood culture, urine culture, and pus culture showed Klebsiella Pneumoniae which was sensitive to Meropenem, so Meropenem was continued. He again developed fever and right ankle swelling which revealed small subcutaneous fluid collection on the medial aspect of the right ankle joint (Figure 2). The swelling measures approximately 2.8x0.9x0.9cm corresponding to a volume of 1cc. It was non-tappable. Orthopedics was taken on board, and they advised to continue conservative management. Due to repeated subcutaneous tissue swellings, the infectious disease team was consulted, and they advised to continue IV Meropenem for 6 weeks due to recurrent abscesses and complicated infection. Flow cytometry was done which revealed low CD4, CD8, and NK cells. Genetics were taken on board for sending a primary immunodeficiency assessment keeping the chronic granulomatous disease in perspective, but the parents refused the assessment due to financial problems. His Hickman line was placed, and counseling was done regarding the care of the central line. Furthermore, parents were advised to hold vaccinations. His Ultrasound kidney at the time of discharge showed a resolution of hydronephrosis.
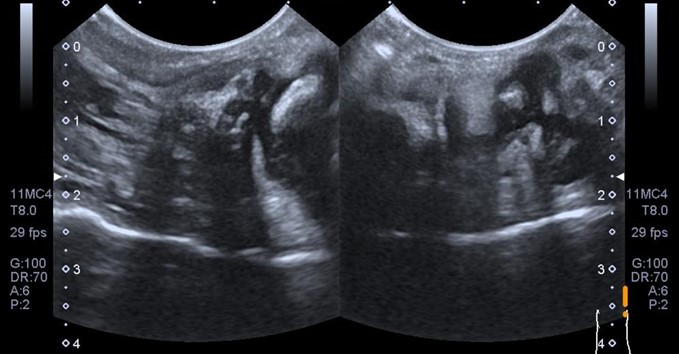
Figure 2. Ultrasound of Right ankle joint showing mild thickening of soft tissue swelling with minimal fluid in the subcutaneous soft tissues.
At 3 months of age, the infant was presented to the Emergency room due to fever, lethargy, and inability to move his left leg for 3 days. He was hemodynamically unstable. The septic workup was sent. He was given boluses and epinephrine support was started. The meropenem, colistin, and vancomycin regime were initiated. MRI of left knee was performed, revealing left knee joint osteomyelitis and associated abscess collection (Figure 3). MRI of left knee joint showed abnormal signals along distal femoral epiphysis predominating involving the posterior lateral aspect of left femoral condyle with adjacent cortical irregularity. An ill-defined collection with enhancing walls was seen in the left knee joint. Collection on the anterior aspect of the femur measured approximately 32 x 11 mm in CC. This collection tracked posteriorly and measured approximately 8 x 4 mm posterior to the lateral femoral condyle. Edematous infiltration of the surrounding soft tissues with post-contrast enhancement of the muscles around the distal femur, representing myositis was also identified. Associated soft tissue edema was also noted. Left Knee Arthrotomy was done. His culture didn't grow any organisms. After he became stable, he has discharged on IV meropenem, oral linezolid, and fluconazole on a 4-week course. During this visit, the parents were convinced to send a primary immunodeficiency workup. After one month, the child came on a follow-up visit and he was thriving well. In addition, his immunodeficiency workup was inconclusive. Therefore, completion of a catch-up vaccination was recommended.
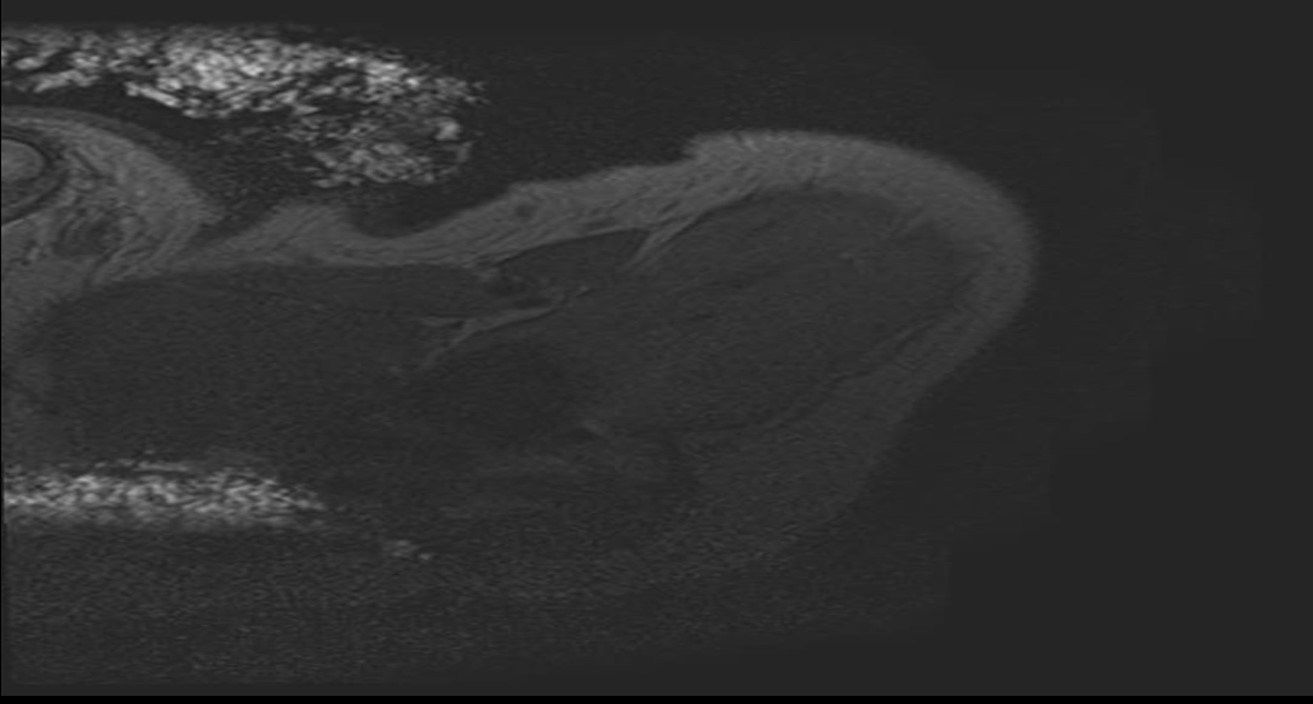
Figure 3. MRI of left knee joint showing osteomyelitis associated collection/ abscess.
Discussion
Circumcision is the surgical removal of the skin covering the head of the penis. It is a relatively safe procedure. Although complications of neonatal circumcision are rare, sepsis, genital mutilation, gangrenous penis, profuse bleeding, permanent disability from the complete or partial amputation of the glans or shaft, the formation of a skin bridge between the penile shaft and the glans, urinary retention, meatal ulcers, meatal stenosis, fistulae, loss of penile sensitivity, dehydration (may result in renal failure), sexual dysfunction and edema of the glans penis have been reported [6]. Circumcision when performed outside the hospital setting by an untrained circumciser is associated with an increase in fatal complications. Therefore, it has been suggested that infectious complications can be reduced with trained and competent practitioners performing the procedure using sterile techniques [7].
In the reported case, the neonate had an early onset Klebsiella pneumoniae infection presented as scrotal swelling followed by right buttock swelling and right ankle abscess on the 8th day of his life. Neonate had no previous history of infection, or direct contact with an infected person, primary immunodeficiency syndrome was also ruled out. All these findings pointed toward the complication of circumcision. In our review, complications due to HSV, syphilis, TB, staphylococcus aureus, streptococcus pneumoniae, and proteus have been found [6-8]. Although fatal complications of circumcision are rare, they should not be excluded. These are some references to the fatal complications of circumcision [9-12]. Most of the cases were presented as sepsis, and multiple and recurrent swellings, as did in our patient. Interestingly, in none of the patients, Klebsiella pneumoniae was isolated. Klebsiella pneumoniae is a gram-negative nosocomial pathogen, transmitted in a hospital or healthcare setting via direct contact (commonly, from patient to patient via the contaminated hands of healthcare personnel) or less commonly via a contaminated environment. This suggested that the route of transmission in our patient is via a contaminated source. Immunocompromised patients and children are at increased risk of Klebsiella Pneumoniae infection.
The clinical manual by the World Health Organization (WHO), discusses male circumcision under local anesthesia and HIV prevention services for adolescent boys and men [13]. Information on basic steps of circumcision such as how to put on and take off surgical gloves, preparing the skin of the genital area of the patient three times, pre-procedure screening, optimal surgical technique based on the level of expertise and patient circumstances, recognizing and responding to adverse events, etc. provides a basis for safe circumcision practice which can be adopted as a Standard of Procedure (SOPs), in various settings providing the service. Evidence based educational sessions are more frequently needed with strict adherence to the SOPs to prevent complications from arising.
Conclusion
Our data demonstrated that fatal complications can be possible if the procedure is not performed properly. It can be reduced by the proper training of the practitioners, sterility during the procedure, and screening of bleeding disorders as a family history of the bleeding disorder can lead to severe post-circumcision bleeding. A child should be discharged home after a thorough medical assessment to treat the child immediately if the complication arises. Additionally, children of more than 2 years of age are at increased risk of complications, this can be avoided by performing circumcision when a child is less than 1 year old. Through these steps, it is possible to improve the safety of this common procedure.
Disclosures
Ethical approval and consent to participate: Written informed consent was obtained from the parents of the patient for the case details to be used for any publication.
Consent to publish: Written informed consent to publish was obtained from the parents of the patient for publication of this case report in a journal as well for other study purposes.
Availability of data and material: Case details are not publicly available because the data is patient medical records but are available from the corresponding author upon reasonable request.
Author’s contribution: AY, RN and WA were involved in the literature search of a topic, introduction, case presentation, case discussion, conclusion, proofreading, and approval of a final version. AM was involved in the manuscript writing, editing and supervision. MAQ was involved in manuscript writing, proofreading, and finalizing.
Conflicts of interest: None
Acknowledgments: None
Funding: None
References
- Hiss J, Horowitz A, Kahana T. Fatal haemorrhage following male ritual circumcision. J Clin Forensic Med, 2000; 7(1): 32-34. doi:10.1054/jcfm.1999.0340
- Baskin LS, Canning DA, Snyder HM, Duckett JW. Treating complications of circumcision. Pediatr Emerg Care, 1996; 12(1): 62-68. doi:10.1097/00006565-199602000-00018
- İnce B, Dadacı M, Altuntaş Z, Bilgen F. Rarely seen complications of circumcision, and their management. Turk J Urol, 2016; 42(1): 12-15. doi:10.5152/tud.2016.78972
- Shabanzadeh DM, Clausen S, Maigaard K, Fode M. Male Circumcision Complications - A Systematic Review, Meta-Analysis and Meta-Regression. Urology, 2021; 152: 25-34. doi: 10.1016/j.urology.2021.01.041
- Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children: a systematic review. BMC Urol, 2010; 10(1): 2. doi:10.1186/1471-2490-10-2
- Tasic V, Polenakovic M. Acute post-streptococcal glomerulonephritis following circumcision. Pediatr Nephrol, 2000; 15(3): 274-275.
- Kirkpatrick BV, Eitzman DV. Neonatal Septicemia After Circumcision. Clin Pediatr (Phila), 1974; 13(9): 767-768. doi:10.1177/000992287401300914
- Distel R, Hofer V, Bogger-Goren S, Shalit I, Garty BZ. Primary genital herpes simplex infection associated with Jewish ritual circumcision. Isr Med Assoc J IMAJ, 2004; 5: 893-894.
- Gairdner D. The fate of the foreskin, a study of circumcision. Br Med J, 1949; 2(4642): 1433-1437, illust. doi:10.1136/bmj.2.4642.1433
- Scurlock JM, Pemberton PJ. Neonatal meningitis and circumcision. Med J Aust, 1977; 1(10): 332-334. doi:10.5694/j.1326-5377.1977.tb76718.x
- King LR. Neonatal circumcision in the United States in 1982. J Urol, 1982; 128(5): 1135-1136. doi: 10.1016/s0022-5347(17)53361-3
- Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics, 1989; 83(6): 1011-1015.
- Manual for male circumcision under local anaesthesia and HIV prevention services for adolescent boys and men. Geneva: World Health Organization, 2018. Licence: CC BY-NC-SA 3.0 IGO.

