Leiomyosarcoma of the Spermatic Cord
Chadli A, Safwate R*, Daghdagh Y, Dakir M, Debbagh A and Aboutaeib R
Department of Urology, IBN Rochd University Hospital Center, Morocco
Received Date: 22/12/2022; Published Date: 13/01/2023
*Corresponding author: Safwate Reda, Department of Urology, IBN Rochd University Hospital Center, Morocco
Introduction
Leiomyosarcomas are rare malignant tumors, they originate from smooth muscle cells with a mesenchymal origin in different structures of the spermatic cord, such as the vas deferens, the wall of the inguinal canal, the blood vessels or the cremaster muscle.
Well-differentiated variants may have a good prognosis; however, high-grade tumors often develop metastases and severely impact patient survival.
Confirmation of the diagnosis requires the use of immunohistochemistry techniques. The treatment of choice is high orchidectomy with ligation of the spermatic cord elements, with the possibility of radiotherapy to reduce the risk of local recurrence.
We report the case of a patient in whom leiomyosarcoma mimicked the symptomatology of a right inguinal hernia.
Case Report
This is a 55-year-old patient, diabetic under oral antidiabetics, asthmatic under treatment, smoking stopped. His symptomatology dates back to 4 months ago with the appearance of a right inguinal tumefaction progressively increasing in volume, which was aggravated by the appearance of pain 1 month before his admission to the urology department. The whole evolving in a context of slight weight loss. Moreover, the patient mistook this mass for an inguinal hernia and did not present any transit disorders, urinary disorders or chronic cough.
Clinical examination found normal vital signs with the presence of a 4 cm mass in the right groin area, slightly painful, mobile in comparison to the deep plane and fixed to the skin, without inflammatory signs in front.
The patient was examined by ultrasound and MRI of the soft tissues, revealing a malignant sarcomatoid tumor in the right inguinal region, measuring 39x35x39 mm with a central cystic area of tumoral necrosis. The tumor displaced and infiltrated the spermatic cord, which remained permeable, and came into contact with the adductor longus and the homolateral corpus cavernosum, and remained distant from the external iliac and common femoral pedicles (Figure 1). An extension workup consisting of a CT scan and a bone scintigraphy was performed, which did not show any secondary lesion apart from an ectopic right kidney in the right iliac fossa and the already known tumor process. The preoperative workup was without particularity.
A high orchiectomy was performed revealing a mass measuring about 4 cm invading the spermatic cord, sparing the superficial femoral vessels, the deep femoral vessels and the saphenous vein.
The diagnosis was confirmed by histopathological examination of the surgical specimen supplemented by immunohistochemical study (H caldesmone) which revealed an intermediate grade leiomyosarcoma with healthy borders (Figure 2).
Focal adjuvant radiotherapy was performed, follow-up was marked by the appearance of multiple pulmonary micronodules on a thoracoabdomino-pelvic scan at 6 months. The patient then received chemotherapy.
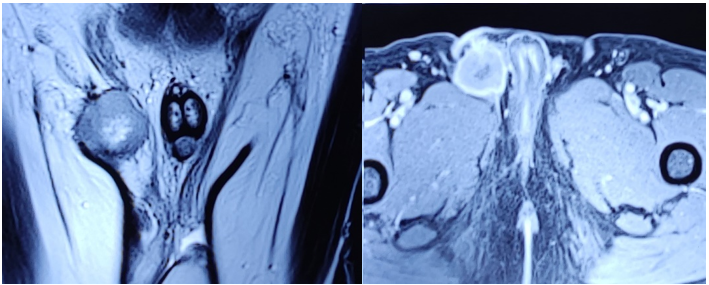
Figure 1: MRI revealing a rounded soft tissue mass in the right inguinal region, with unclear irregular boundaries, T1 hyposignal, T2 intermediate hypersignal with heterogeneous enhancement delimiting a central cystic area of tumor necrosis.
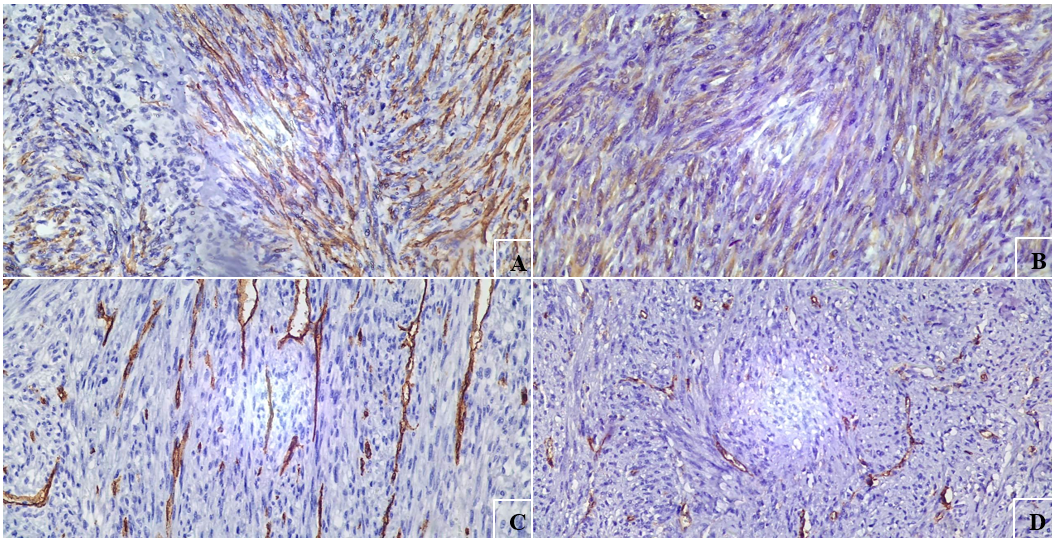
Figure 2: Tumor cells express AML (A) and H Caldesmone (B) but do not express CD34 (C) nor Desmin (D).
Discussion
In the group of paratesticular tumors, spermatic cord location is the most common and represents 75% of the whole group. The majority of spermatic cord tumors are benign lipomas, however, when they are malignant most of them are sarcomas and this is because the embryological origin of the spermatic cord is mesodermal [1]. Liposarcoma is the most common type of sarcoma found in the retroperitoneum and inguinoscrotal region, only 0.1% of leiomyosarcomas appear as inguinal hernias and occur in the inguinal region [2].
Leiomyosarcomas are classified into 4 histological subtypes: well-differentiated, myxoid, pleomorphic, dedifferentiated; they may arise from spermatic cord tissue which represents an extension of retroperitoneal fat or a malignant transformation of a pre-existing lipoma or leiomyosarcoma. These tumors occur more often in adults than in children, with extremes of age ranging from 16 to 90 years and an average age of 56 years [3] (vukmurovik).
Preoperative diagnosis of these leiomyosarcomas is difficult, as clinicians are not accustomed to seeing inguinoscrotal tumors simulating the symptomatology of inguinal hernias and this is due to the low prevalence of tumors at this location compared to hernias and other pathologies (hydrocele, spermatocele, orchitis, epididymal tumor and cyst).
Clinically, leiomyosarcoma of the spermatic cord appears as a solid, firm mass in the inguinal canal or scrotum, most often unilateral, and gradually increasing in size. It is distinct from the testis and may be accompanied by pain, hydrocele, or symptoms secondary to metastases. Patients normally complain of a feeling of scrotal compression or heaviness in the scrotum [1-3].
Ultrasound is the first-line radiological examination in case of inguinoscrotal abnormality, it can identify the location of the mass and the state of the testis and spermatic cord as well as distinguish intratesticular masses from extratesticular masses. Leiomyosarcoma appears as a regular, vascularized, hyperechoic and heterogeneous mass with areas of necrosis and a soft tissue contingent of variable size and may compress the testis and surrounding structures [4]. Ultrasound is complemented by CT and MRI which are more specific to the study of tumor masses. The CT scan allows to localize the tumor with more precision and to study its morphology, its characteristics, its extension to the neighboring elements and the search for secondary localizations (lungs, adenopathies). MRI is the gold standard for sarcoma imaging, it is the most specific for the study of local extension [3].
It is important to know the routes of dissemination of these lesions for a better therapeutic approach, leiomyosarcomas tend to migrate by the lymphatic route first, then the hematogenous route and from step to step invading the surrounding tissues [5].
Due to the rarity of spermatic cord tumors, there is no consensus regarding the management and therapeutic strategy for these lesions. Most scientific societies recommend radical orchiectomy with high spermatic cord ligature as treatment for a malignant testicular mass with the major goal of resection of the mass to R0 healthy margins [6]. Local recurrence is common in leiomyosarcomas and depends on tumor differentiation, type and size. Given the radiosensitivity of leiomyosarcomas, some authors recommend adjuvant radiotherapy that should cover the internal inguinal orifice, the specific survival at 5 years was 80% and no local recurrence was detected. The use of chemotherapy is reserved for high-grade tumors or in case of metastatic disease.
Conclusion
Spermatic cord tumors are very rare, most of them are benign tumors, sarcomas represent the malignant tumors. Preoperative diagnosis is difficult due to the low prevalence of these tumors at this location. CT and MRI are the 2 radiological examinations of choice. Treatment is based on orchiectomy with high ligation of the spermatic cord and wide excision of surrounding tissues. Adjuvant radiotherapy is required to avoid local recurrence.
References
- Moschini, Marco, et Agostino Mattei. « Diagnosis and Management of Spermatic Cord Tumors ». Current Opinion in Urology 27, no 2017; 1: 7679.
- Montgomery E, et R Buras. « Incidental Liposarcomas Identified during Hernia Repair Operations ». Journal of Surgical Oncology 71, no, 1999; 1: 5053.
- Vukmirovic Filip, Nihad Zejnilovic, et Jovan Ivovic. « Liposarcoma of the Paratesticular Tissue and Spermatic Cord: A Case Report ». Vojnosanitetski Pregled 70, no, 2013; 7: 69396.
- Frates MC, Benson CB, DiSalvo DN, Brown DL, Laing FC, et PM Doubilet. « Solid Extratesticular Masses Evaluated with Sonography: Pathologic Correlation ». Radiology 204, no, 1997; 1: 4346.
- Patel R, Chana P, Armstrong J, et R Lawrence. « Leiomyosarcoma of the Inguinal Canal ». The Annals of The Royal College of Surgeons of England 96, no, 2014; 6: e89.
- Vagnoni Valerio, Eugenio Brunocilla, Riccardo Schiavina, Marco Borghesi, Giovanni Passaretti, Giorgio Gentile, et al. « Inguinal Canal Tumors of Adulthood ». ANTICANCER RESEARCH, 2013; 8.

